Liver and Risks of Vitamin A Toxicity
I share this blog post even though I knew there would be some backlash. But I’m a big girl (and I have my faith) and know that my heart is in the right place to share this information.
If you have no idea what I’m talking about, I shared a YouTube and Podcast interview with Grant Genereux on the concerns of vitamin A toxicity and how liver (even kidneys) is a great (sometimes too much) source of vitamin A.
In hindsight, I realize I shouldn’t have used such a bold statement on the YouTube thumbnail and that is my fault. For that, I apologize if it took away from my message. And for the record, I’m not doing this for any other reason than to share that some people can adversely be affected by consuming too many foods and products that contain vitamin A. And frankly, also to reduce some of the guilt I feel for advocating for frequent liver consumption.
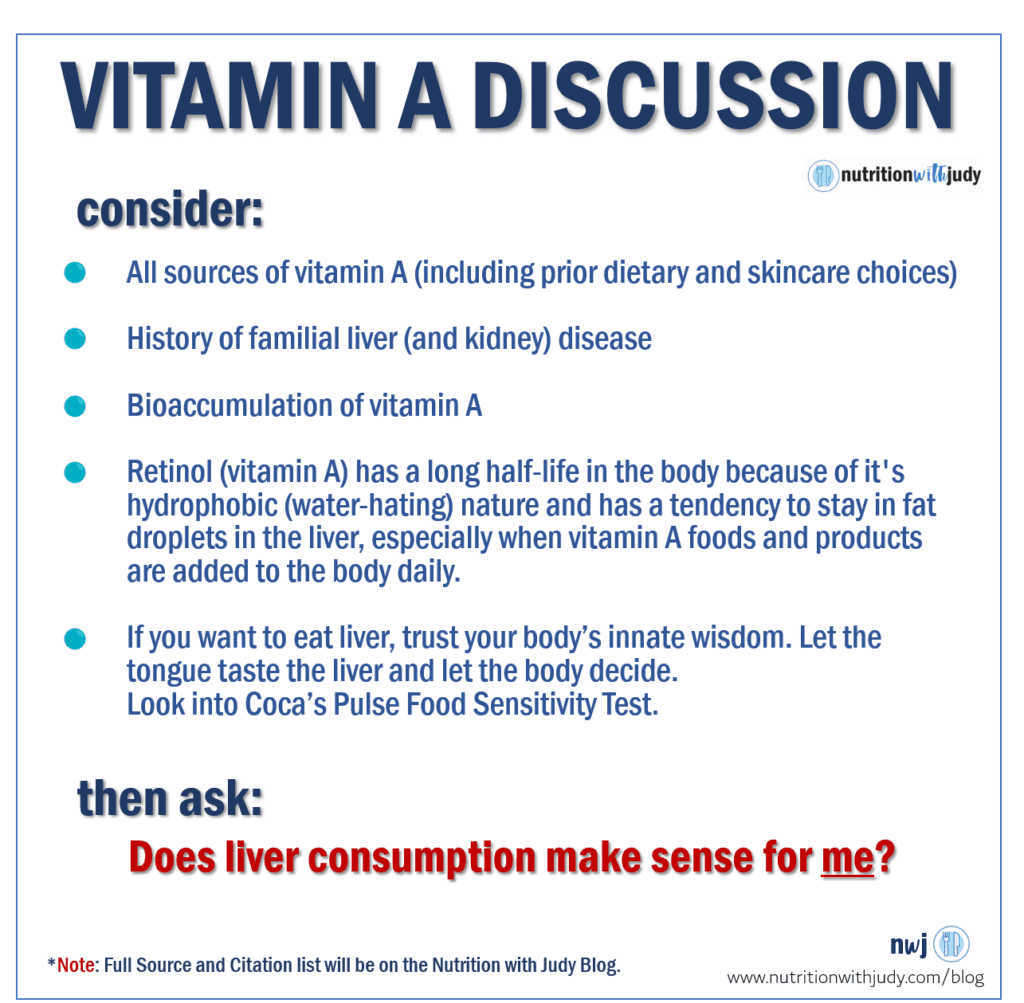
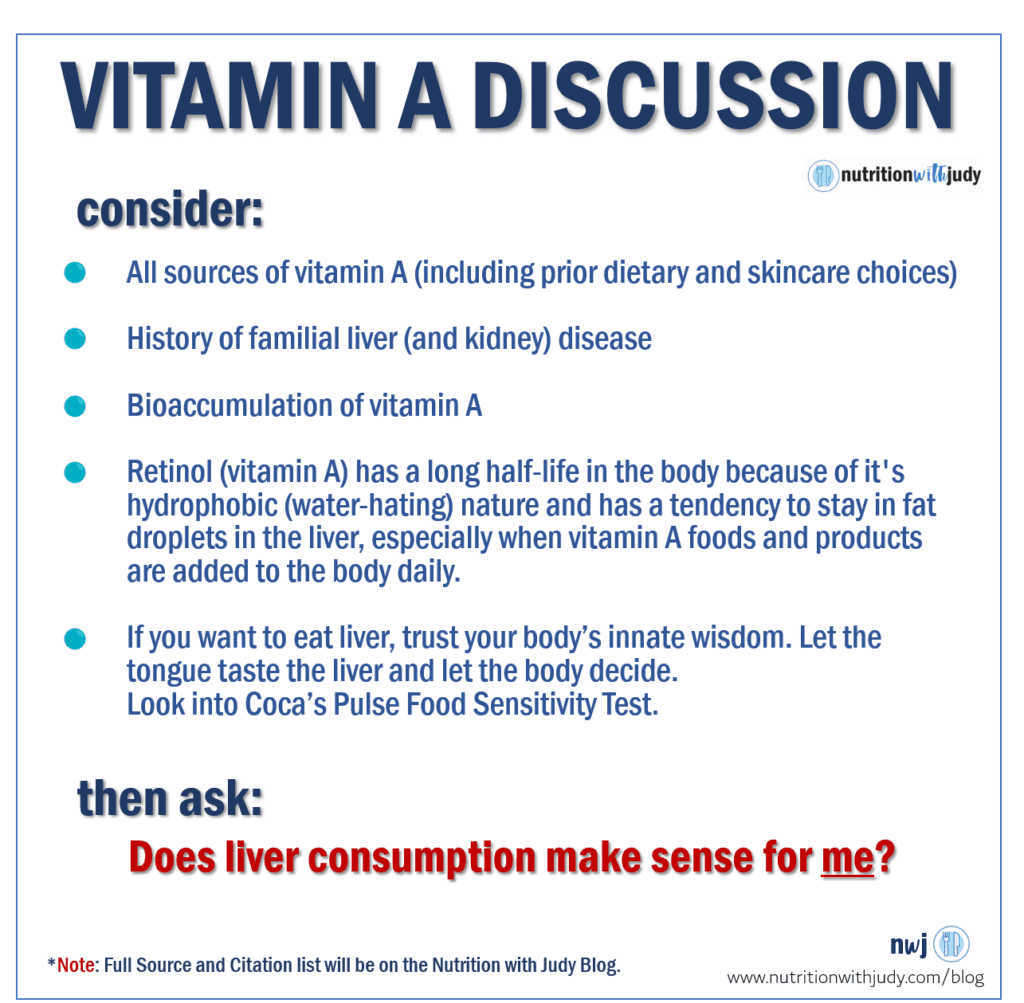
If we’re predisposed to different genetics, life circumstances, and illness, we know that for some of us following a meat-based diet, one of the many foods that can be a tipping point to excess vitamin A (to a point of toxicity) is liver (maybe even kidneys).
Not everyone has to remove liver from their diet but for what I share and for my family and clients, I will always proceed with caution before sharing anything related to liver consumption. Considering all things, the risks of too much vitamin A now outweigh the rewards of liver’s nutrient density.
Nutritional Mins and Maxs
If you are mostly meat-based, you personally understand that we may not have to meet the daily requirements of all essential vitamins and minerals (e.g., vitamin C).
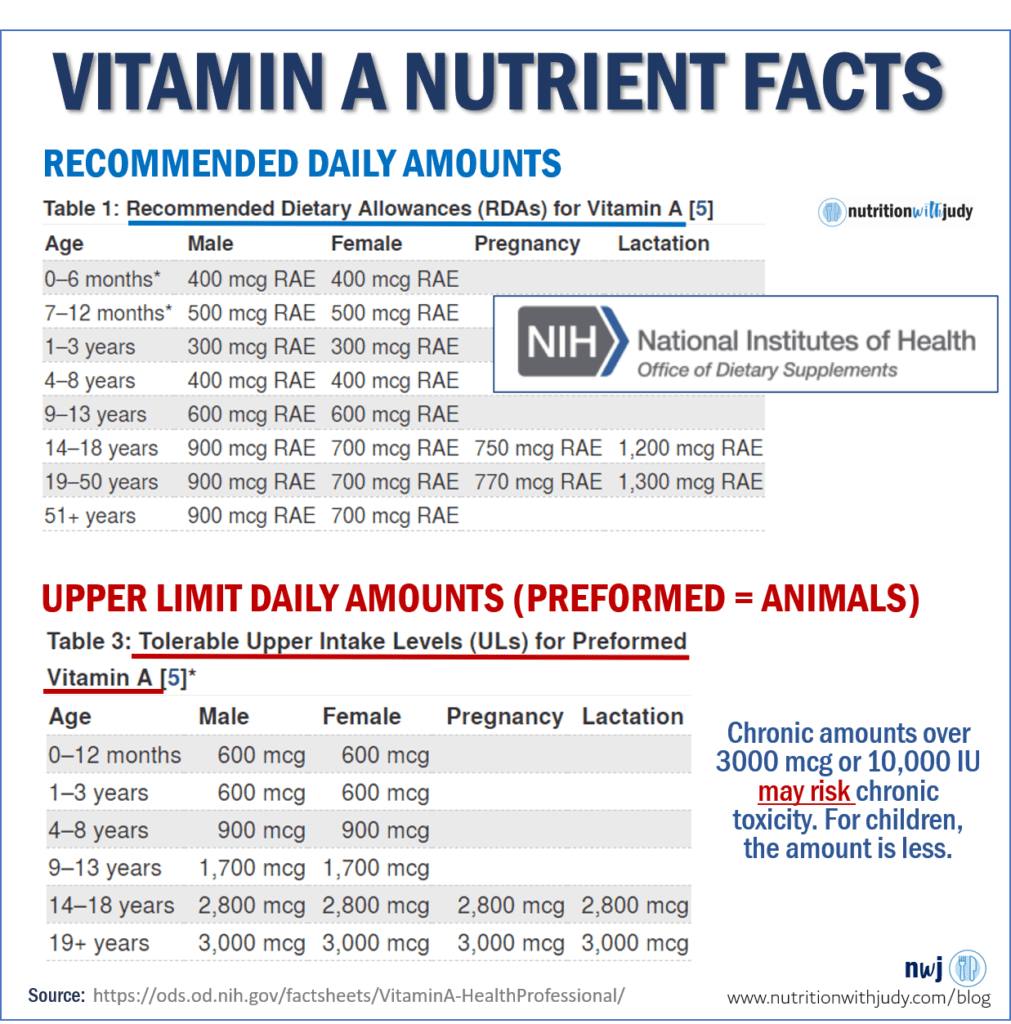
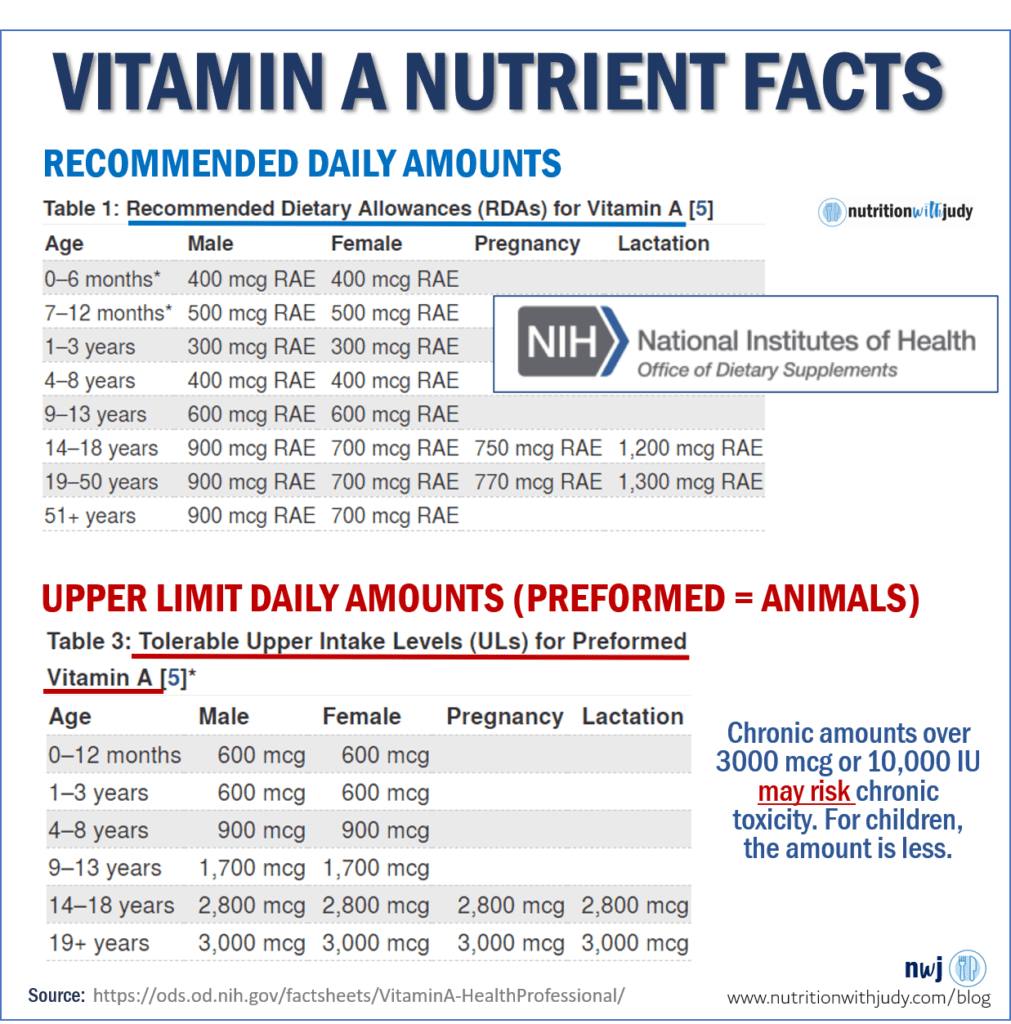
But what about the max? The Tolerable Upper Limits are defined by various types of studies (epidemiological, population, depletion, and repletion studies)
The Food and Nutrition Board (FNB) and National Academies define tolerable upper intake levels by “the highest level of nutrient intake to pose no risk of adverse health effects for almost all individuals in the general population. As intake increases above the UL, the risk of adverse effects increases.” You can read more here.
Sure, the minimum requirements and even upper limits may be incorrect. But stretching past the upper limits and knowing that there are risks of vitamin A overconsumption, it doesn’t seem like a worthwhile risk.
There are different forms of vitamin A and for this discussion, I’m primarily focusing on the preformed, retinol or animal forms.
- Per the NIH of Dietary Supplements: The FNB has established ULs for preformed vitamin A that apply to both food and supplement intakes.
- The FNB based these ULs on the amounts associated with an increased risk of liver abnormalities in men and women, teratogenic effects, and a range of toxic effects in infants and children.
- The FNB has not established ULs for beta-carotene and other provitamin A carotenoids.
Plant-based carotenoids will be better absorbed in the small intestine with fats or if the plant is cooked. But for this discussion, we will assume there is almost no vitamin A from plant-based foods (other than the vitamin A that has accumulated in the liver over the years).
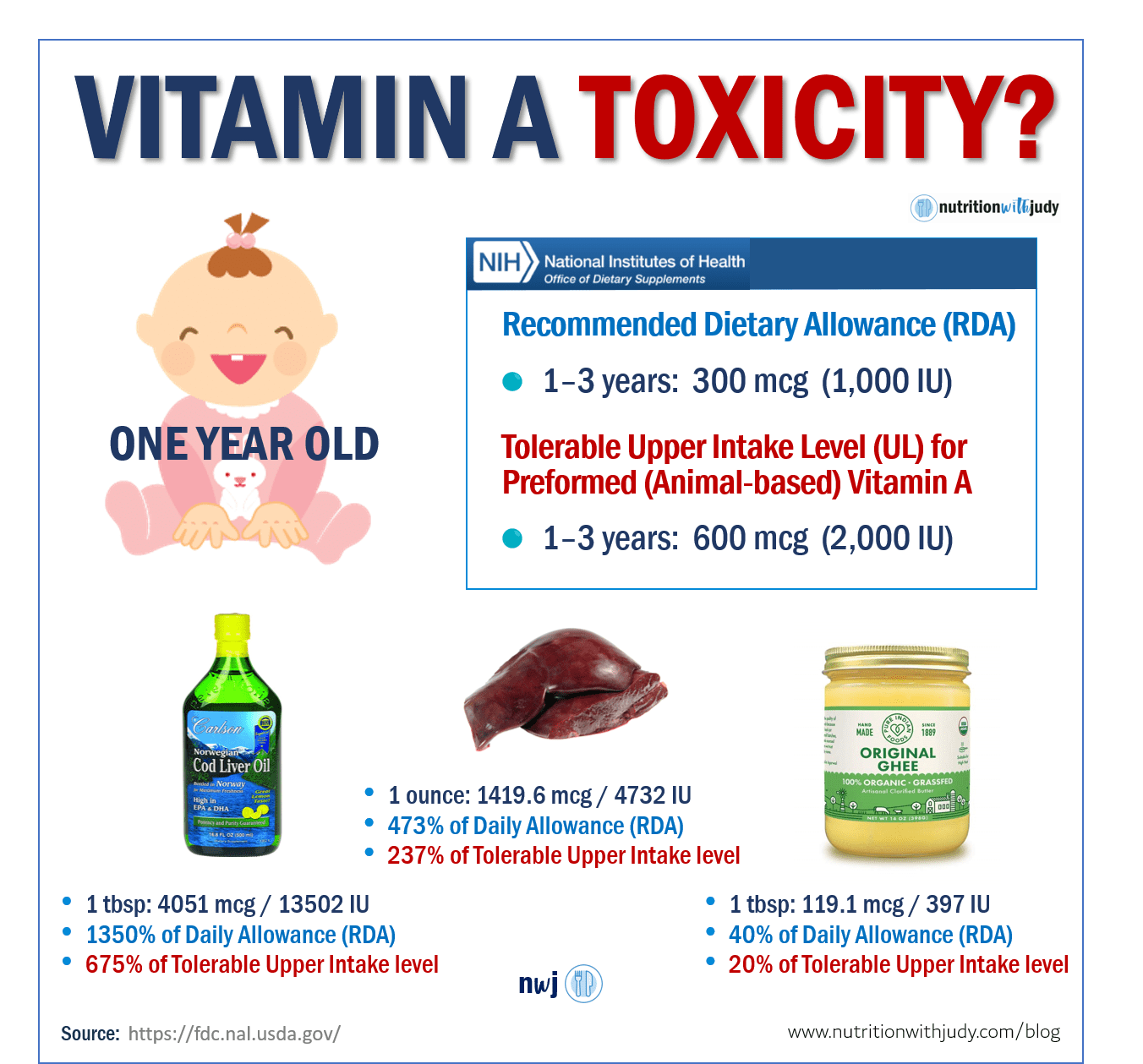
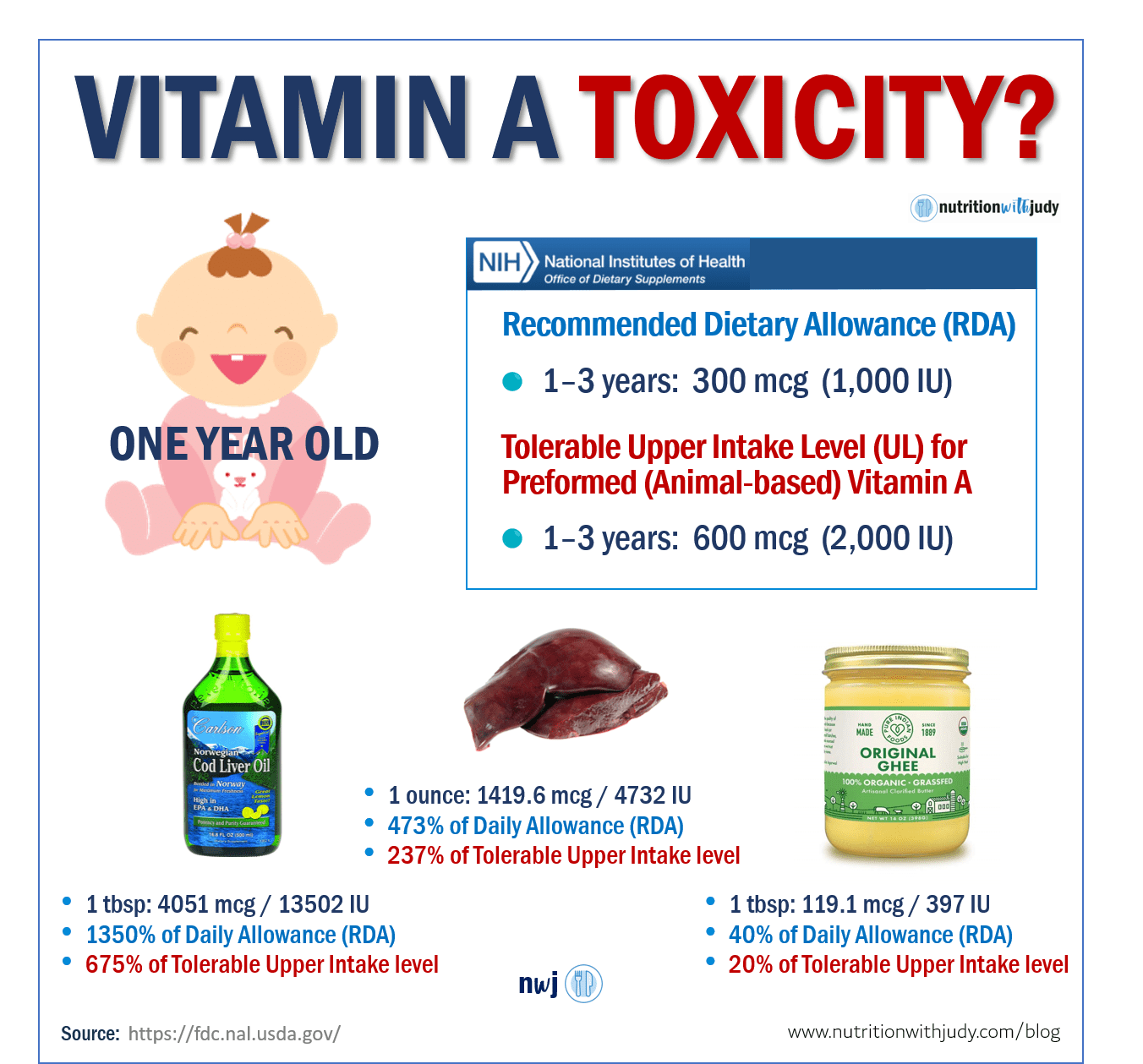
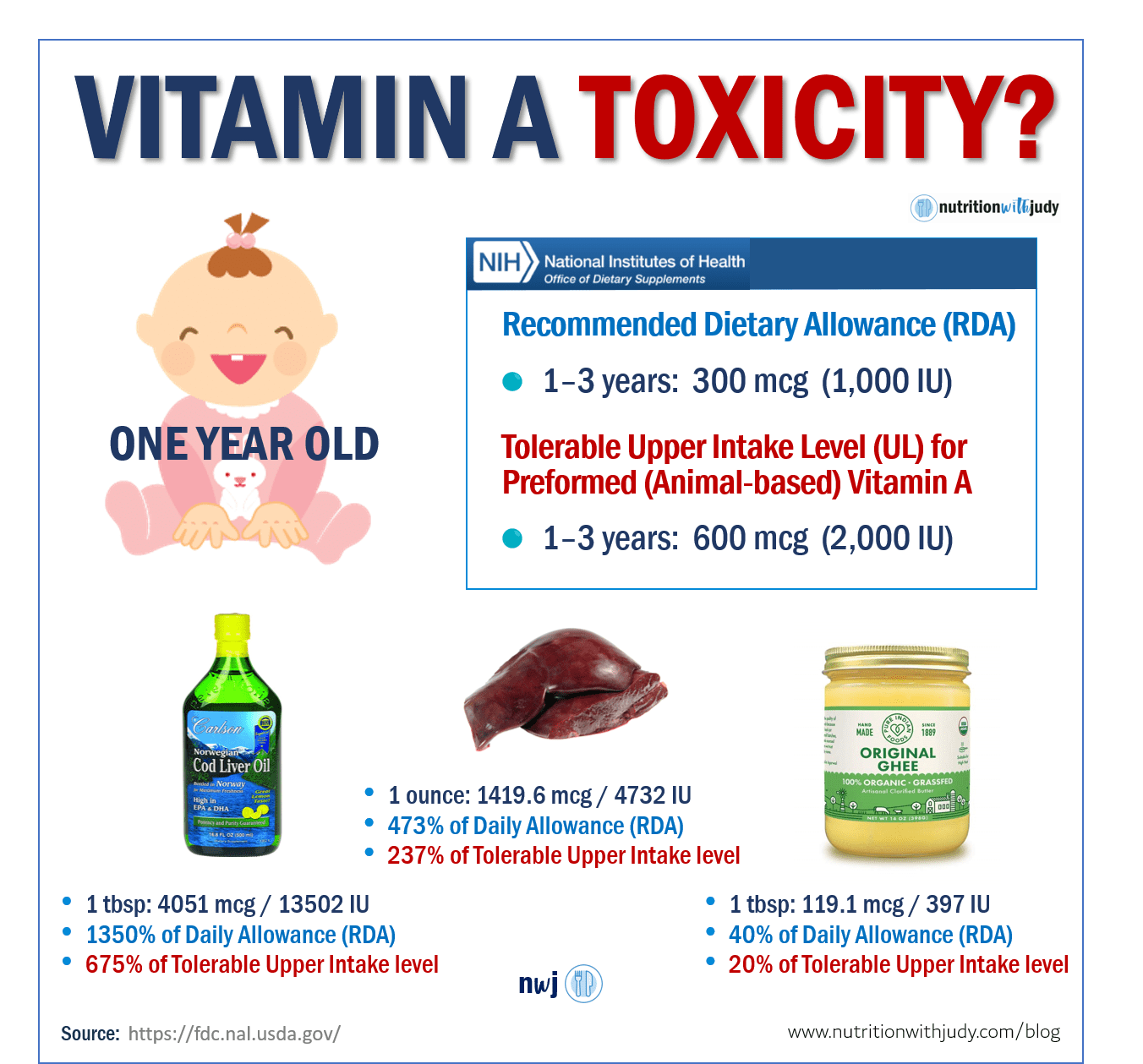
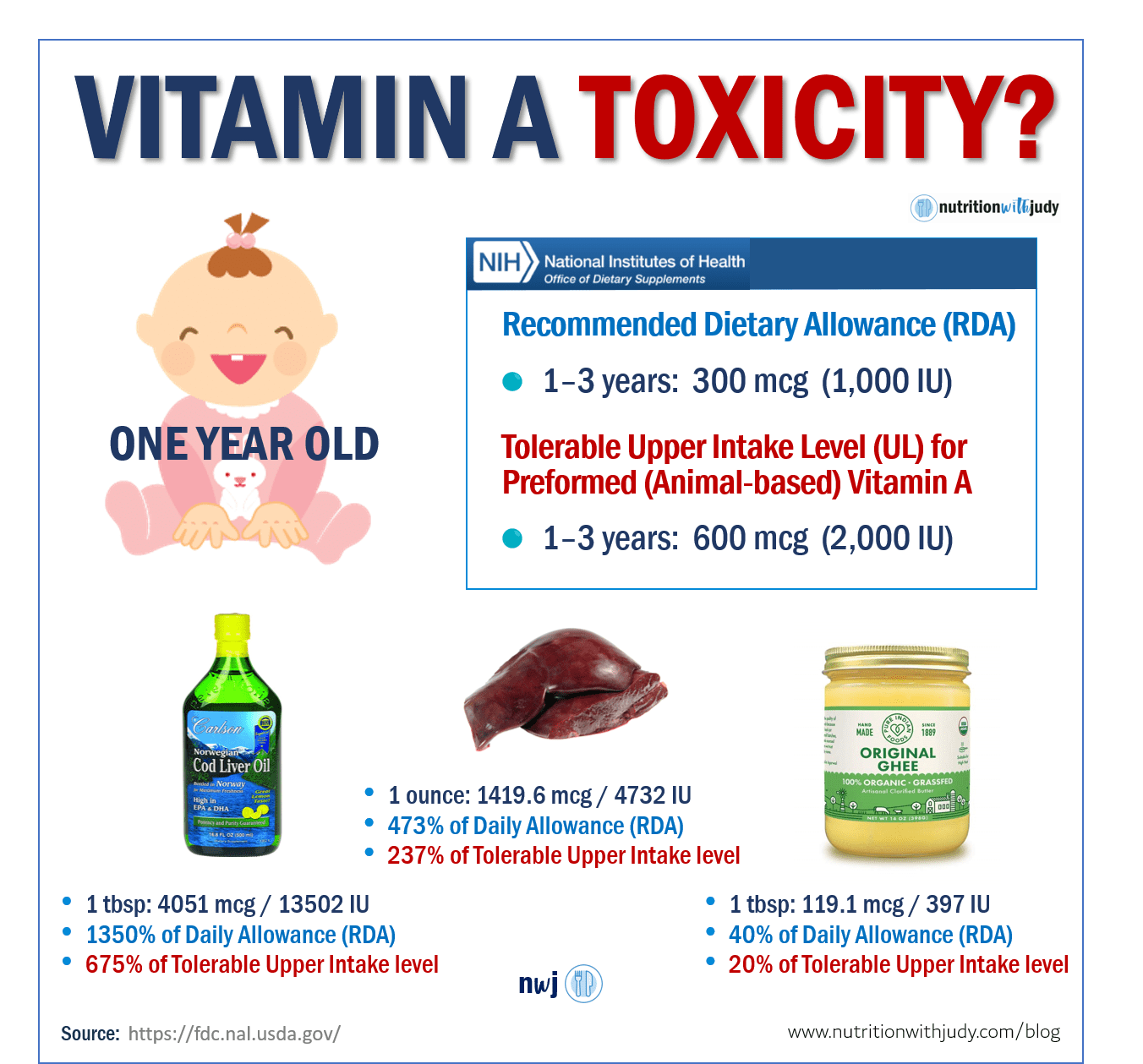
Case Study: Children Ages 1 -3
For a child between the ages of one and three, the RDA is 300 mcg or 1,000 IU and the tolerable UL of 600 mcg or 2,000 IU. This again is for the preformed (animal variety) vitamin A.
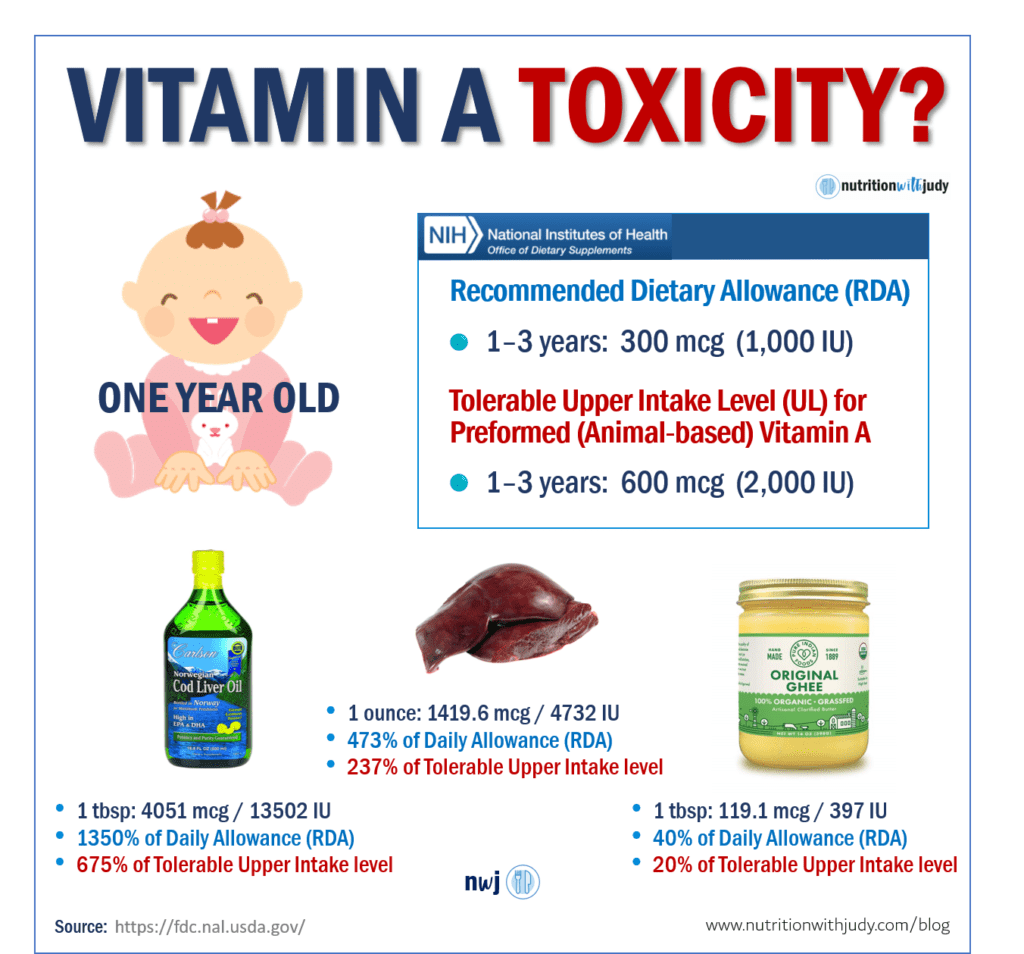
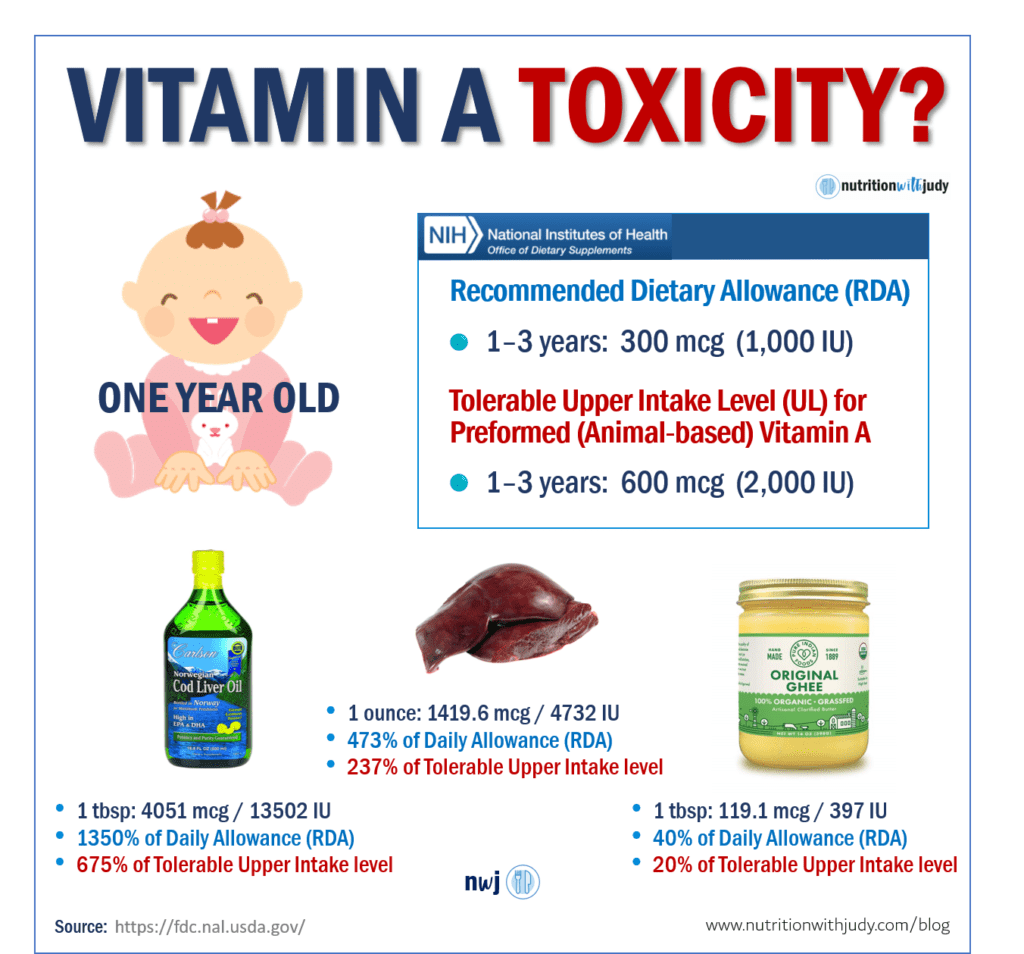
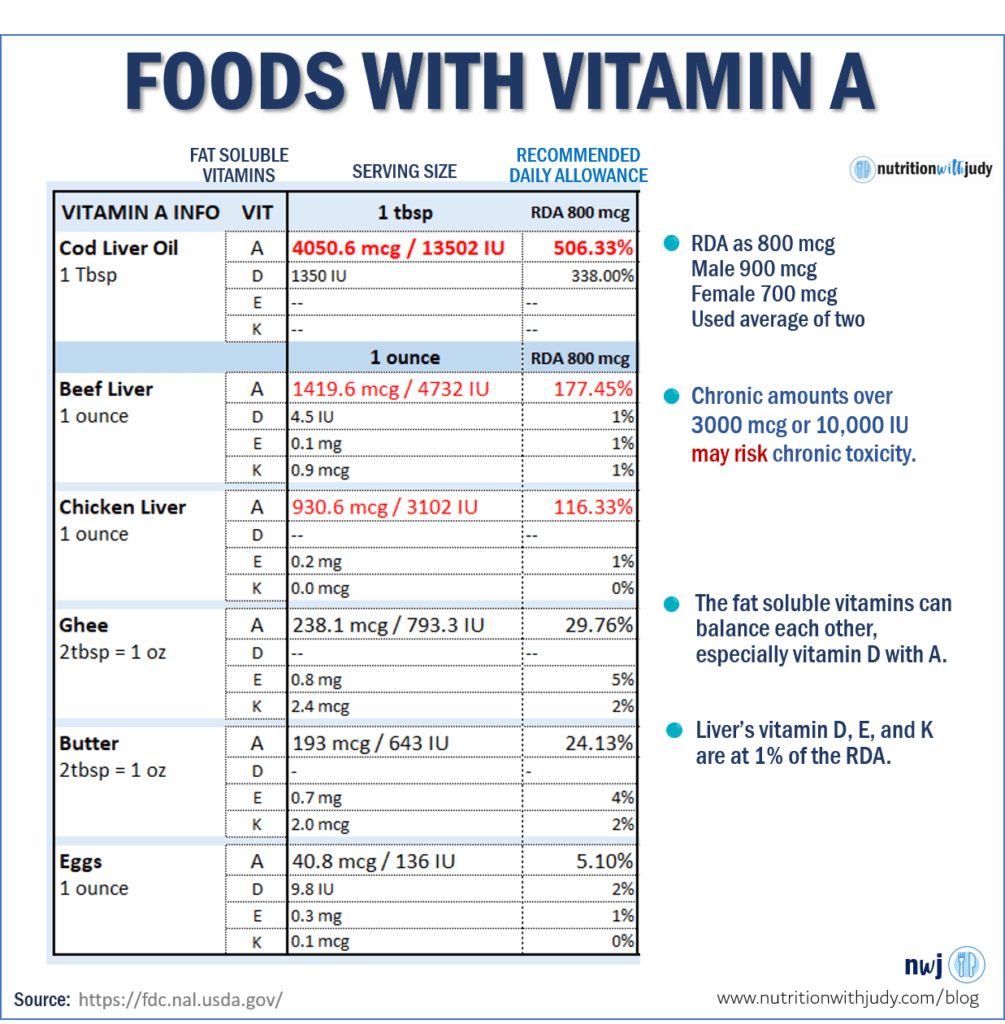
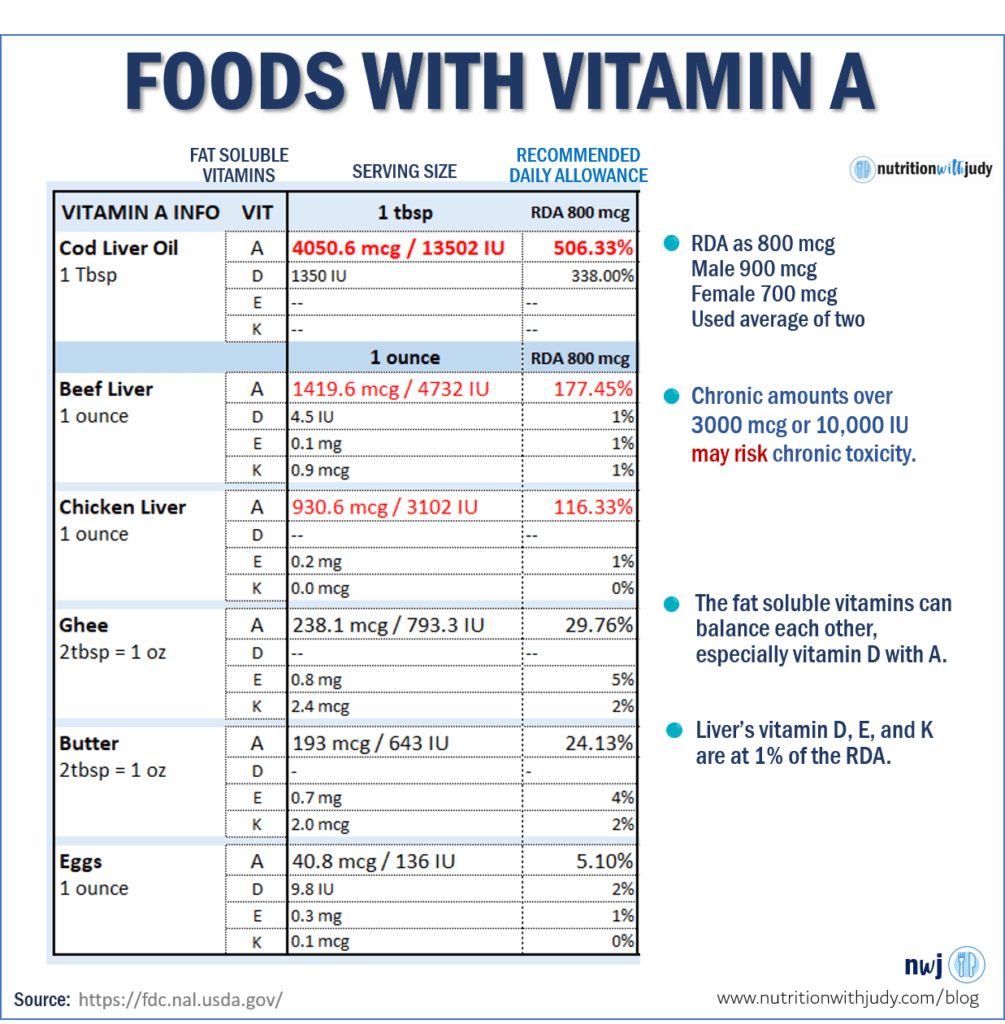
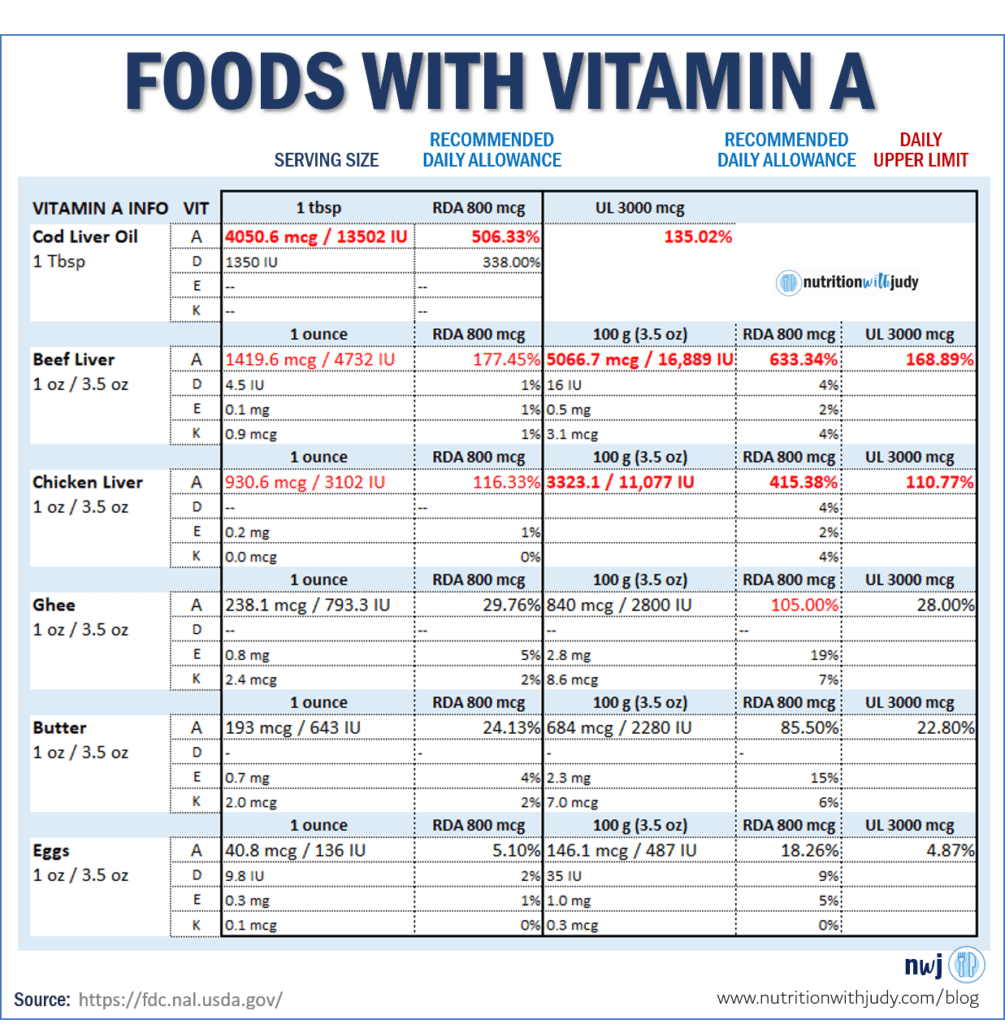
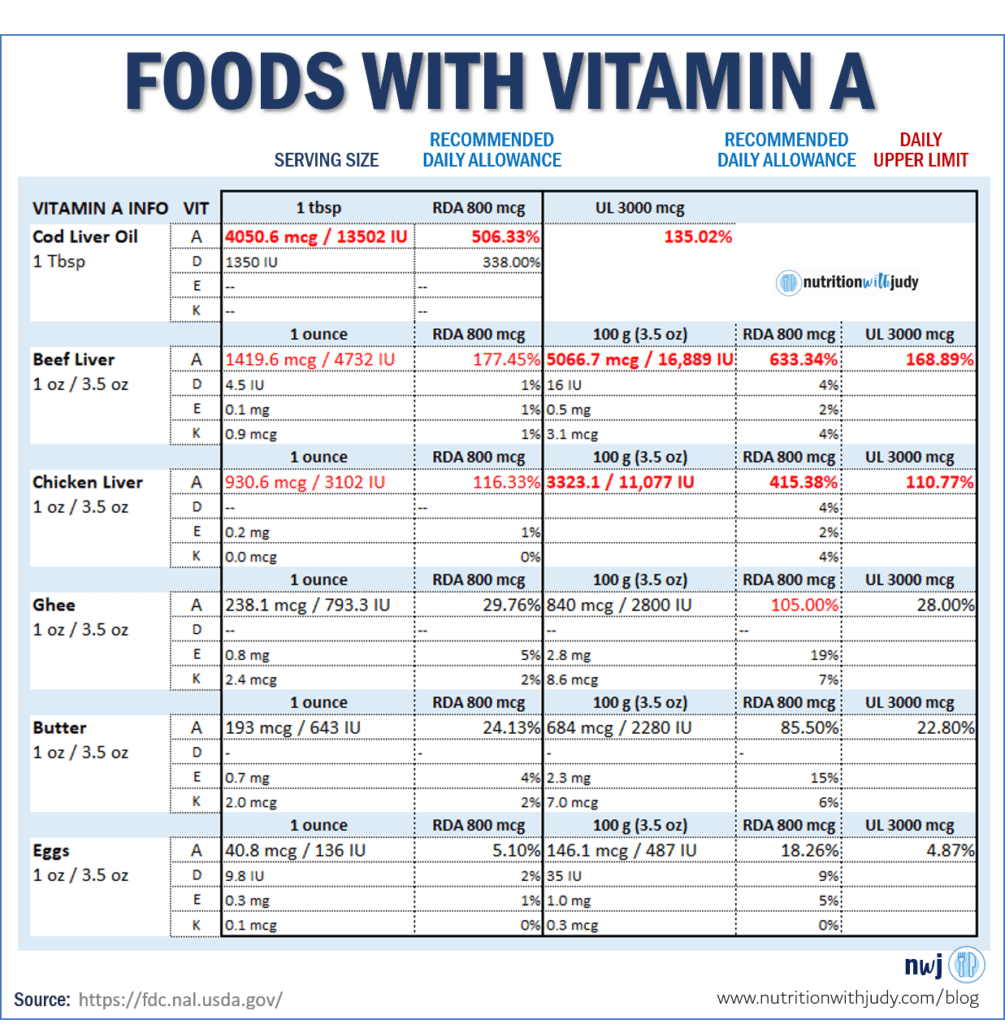
If you consider cod liver oil, beef liver, and ghee, from a purely mathematical point of view, cod liver oil and beef liver far exceed the tolerable upper intake levels.
So what happens if we keep surpassing the upper limits daily, especially in a child where the liver’s total functioning capability is not developed until age two or three? You can read about a child’s liver development timeline, here and here.
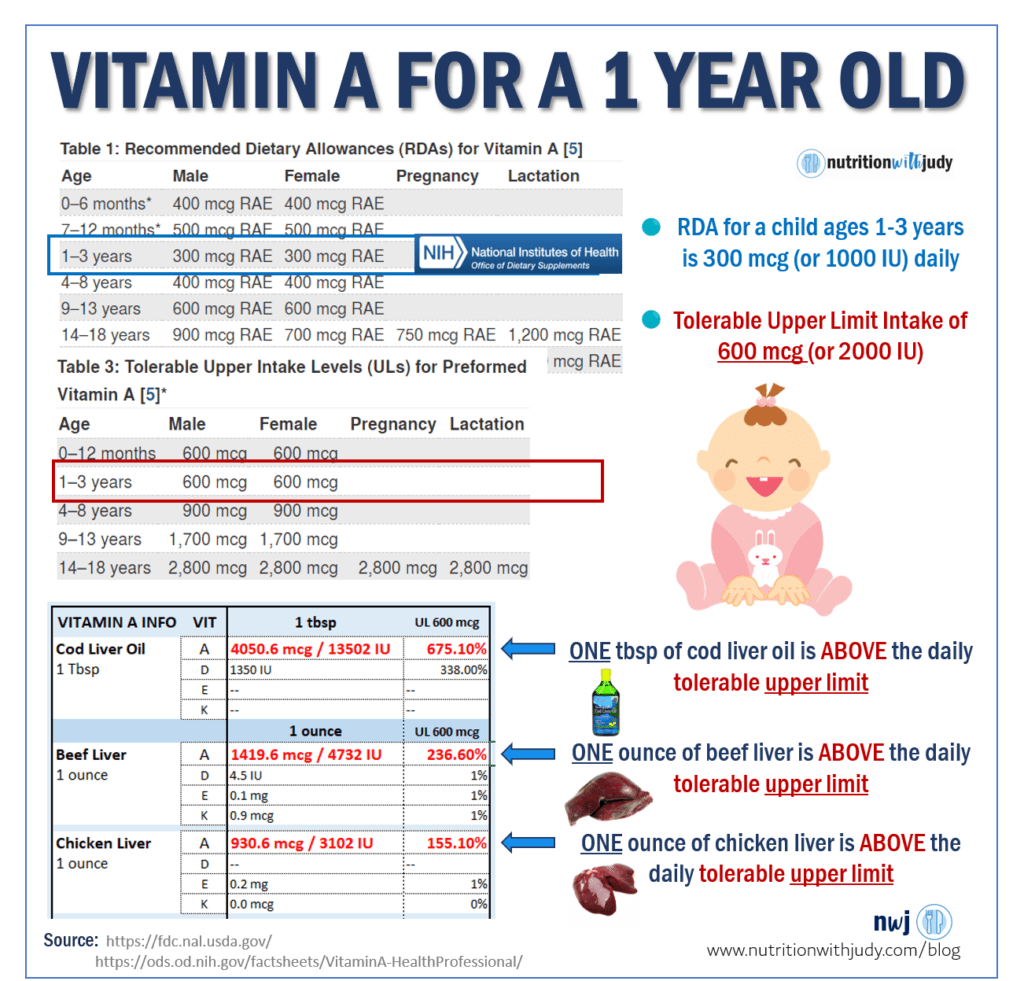
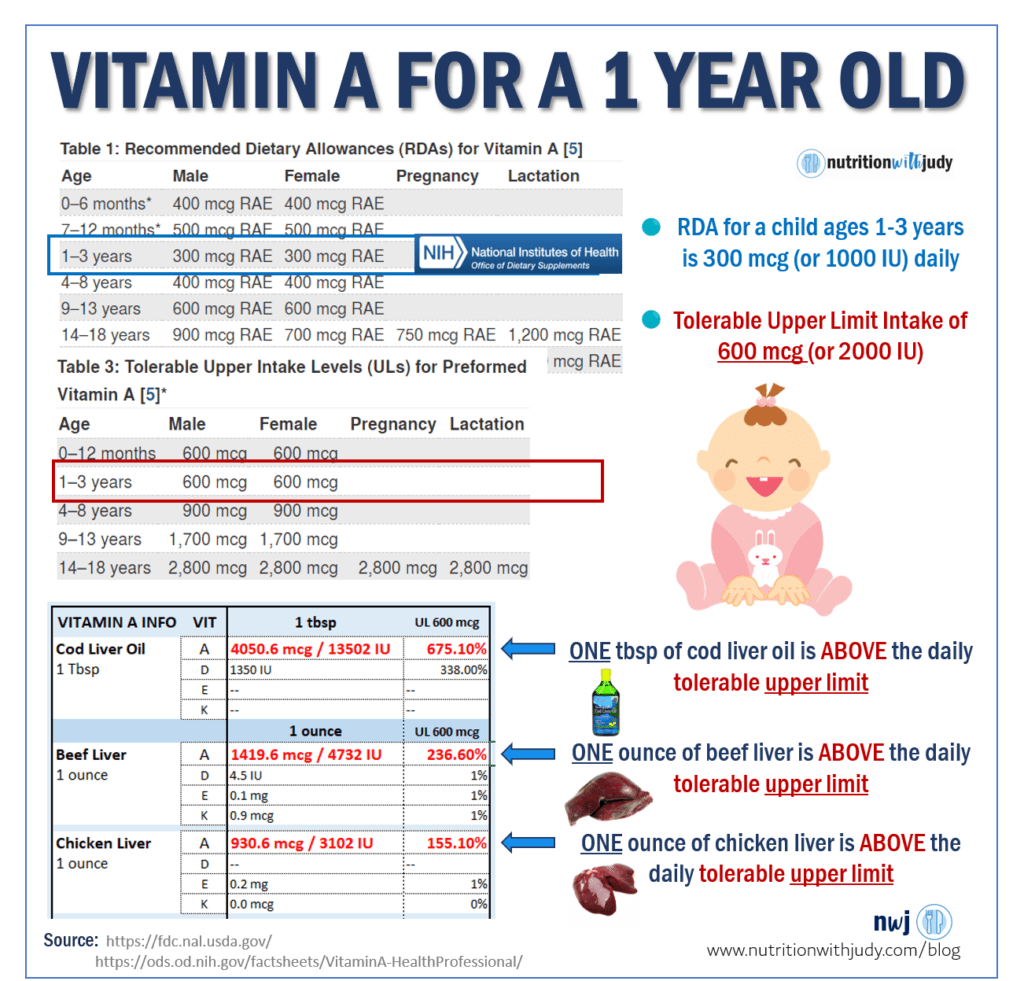
So for a one to three-year-old, one ounce of beef (or chicken) liver exceeds the UL threshold for daily vitamin A. Again, these upper limit amounts can be disputed but I personally would never recommend my clients to take that risk with their young child.
I wouldn’t take that risk with my own children, especially when they also eat other vitamin A-rich foods like butter, dairy, and eggs. And in case you didn’t know, almost all store-bought dairy is fortified with vitamin A (and D), especially the low-fat and reduced-fat varieties. You can read more here and here. Even if a dairy cow is pasture-raised and grass-fed, if the dairy is reduced-fat, it has been fortified.
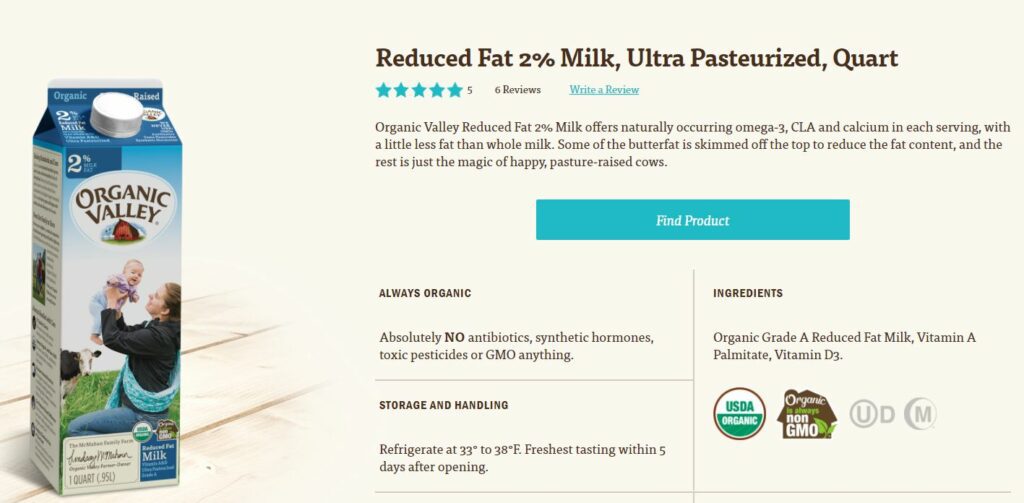
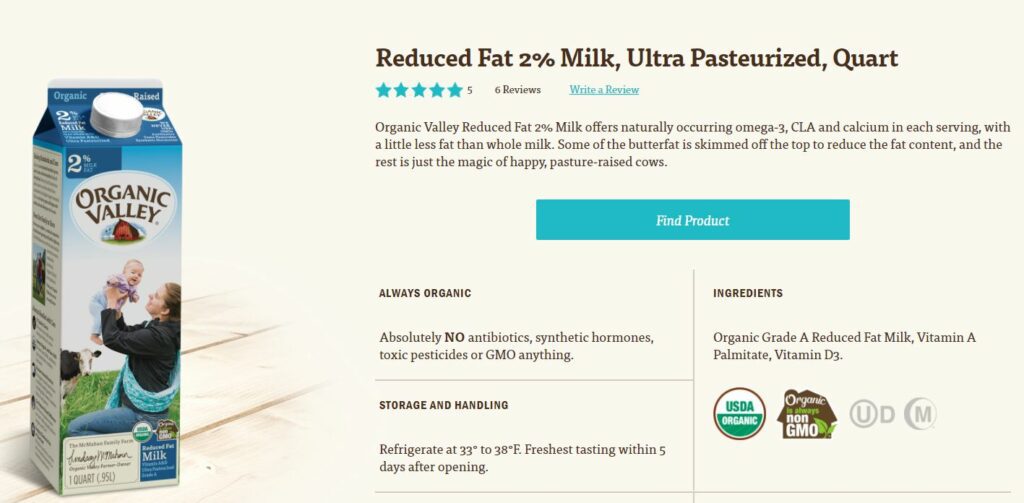
Image Source: Organic Valley
I applaud Organic Valley for sharing vitamin A palmitate and vitamin D3 as separate ingredients as they add these synthetic vitamins to their milk (by law). Not all food companies share this on their labels.
You can read more about the governing bodies and the requirements of fortified vitamin A and D here, here, here, here, and here.
On a tangent, if you are supplementing vitamin D, consider all vitamin D sources you’re adding to your diet (including fortified foods). If you want to read my post on why raw milk is best, you can find it here.
Kerrygold butter is extra golden because of the beta-carotene in the dairy cow’s diet. This simply means that there is more vitamin A in every bite of butter. The same holds true for grass-fed cows and their fat. While the vitamin A is minimal, it is still more than conventional cow fat, assuming these cows were not fed grains with supplemental vitamin A.
So if your child consumes foods with higher vitamin A amounts, the one ounce of liver becomes that much more worrisome, in terms of vitamin A overload.
Case Study: Adults 18+
For adults, the RDA for males is 900 mcg and for females at 700 mcg. The tolerable UL for both males and females is at 3,000 mcg or 10,000 IU. For simplicity, I made the RDA at 800 mcg, averaging the amount for males and females.
You can see that 1 tablespoon of cod liver oil or one ounce of beef or chicken liver exceeds the RDA without any additional food. If you add butter or ghee while cooking your liver, or add butter or ghee to make pâté, you’re well on your way to the UL amounts.
And this is just one ounce of beef liver.
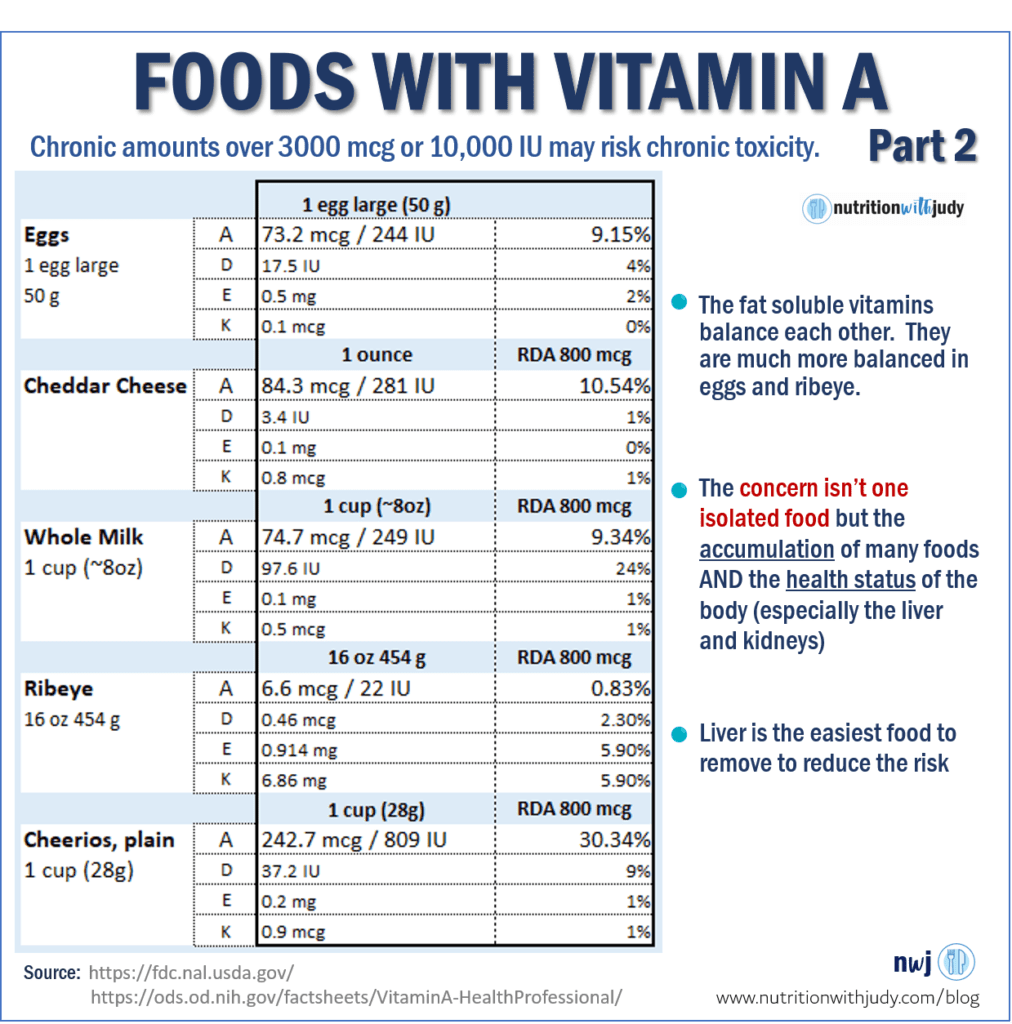
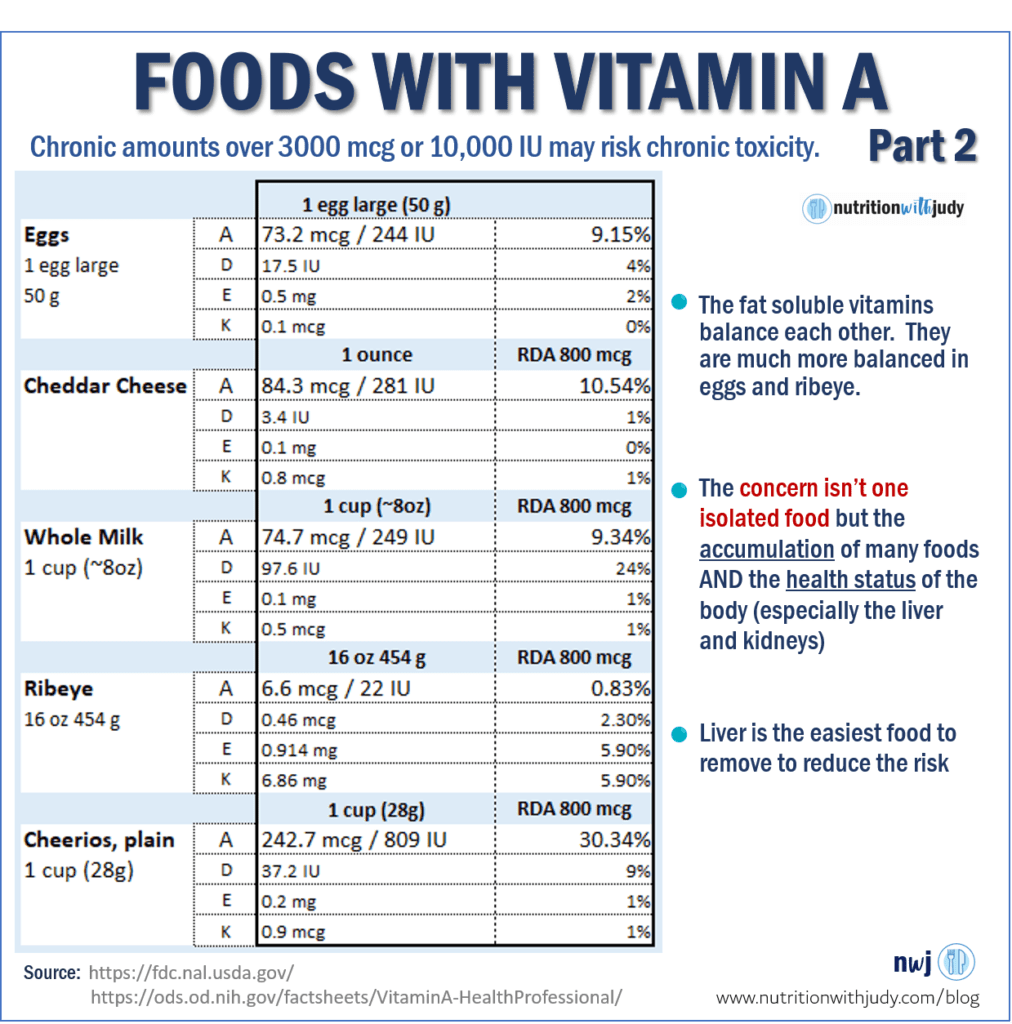
Part of the issue is not because of liver specifically, but the fact that we are fortifying all our grains, cereals and dairy with synthetic vitamin A. Who would have thought that 1 cup of plain cheerios would have 243 mcg or 30% of an adult’s recommended allowance of vitamin A?
We are also taking supplements with added vitamin A. At one point we thought we were deficient in vitamin A and we tried to correct it by fortifying our foods with synthetic vitamin A. I don’t think they considered that we may eat a variety of these foods that would then cause high amounts of vitamin A in the body.
The fat-soluble vitamins (A, D, E and K) work together. I cite some examples in Carnivore Cure. Vitamin D is supposed to offset some of the vitamin A toxicity concerns. But if we think of natural foods, liver barely has any vitamin D (or vitamins E and K for that matter).
So how are we offsetting the high amounts of vitamin A in liver? The sun?
Below is the tolerable UL for 3.5 ounces of beef and chicken liver. Both exceed the tolerable upper limit. Maybe we don’t eat 3.5 ounces but are you certain there are no other vitamin A foods in your diet?
Some people recommend that 1 to 2 ounces daily is safe. That means they are abiding by the daily tolerable upper limits as two ounces of just beef liver technically is still a hair under the 3,000 mcg or 10,000 IU tolerable upper limit amount. But the logic is questionable as most people still consume other foods that contain vitamin A.
And if these people agree with the daily tolerable upper limits, why are they limiting consumption to two ounces? Shouldn’t they advocate for more as there’s no supposed risk to natural food forms of vitamin A?
Meat-Based Vitamin A Meal
While most standard American dieters don’t eat 5 eggs in one meal, many meat-based eaters do. Maybe it’s not even in one meal, but the amount of vitamin A foods shown below is pretty commonplace in the meat-based Carnivore communities.
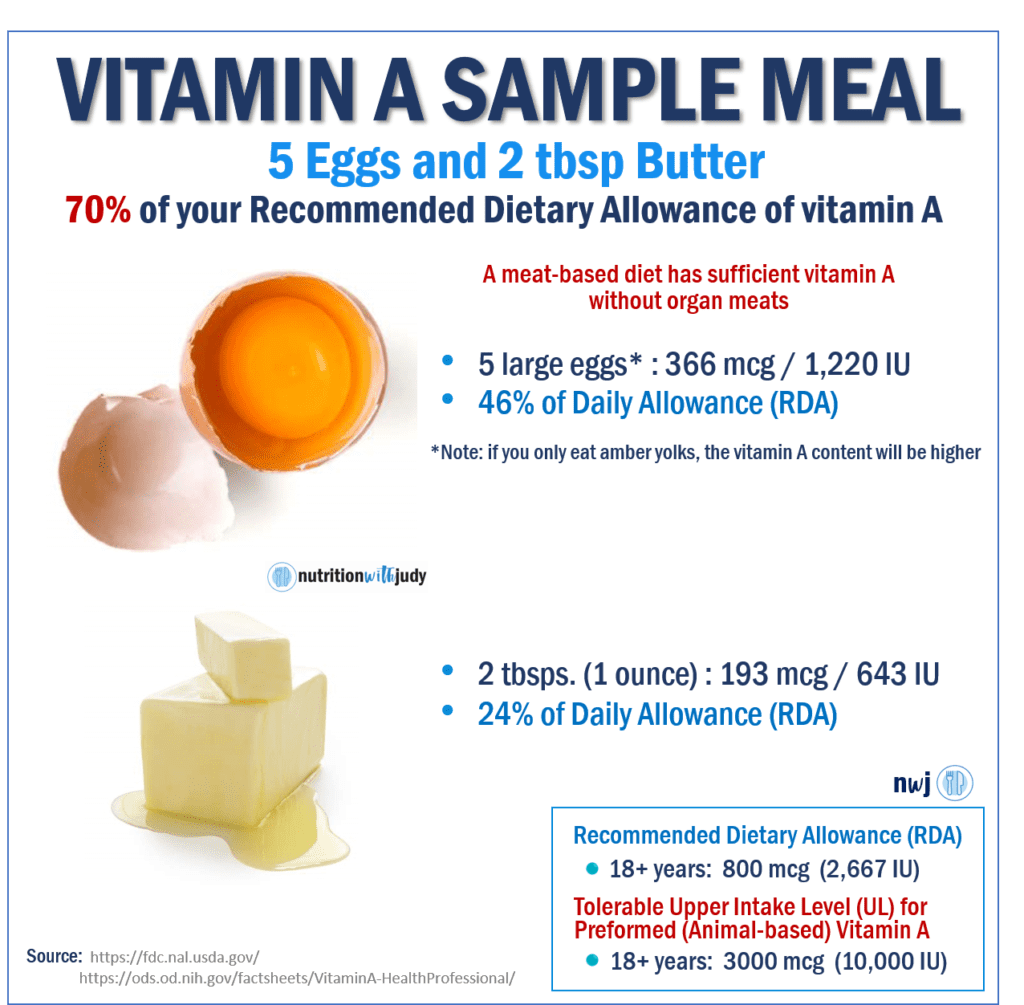
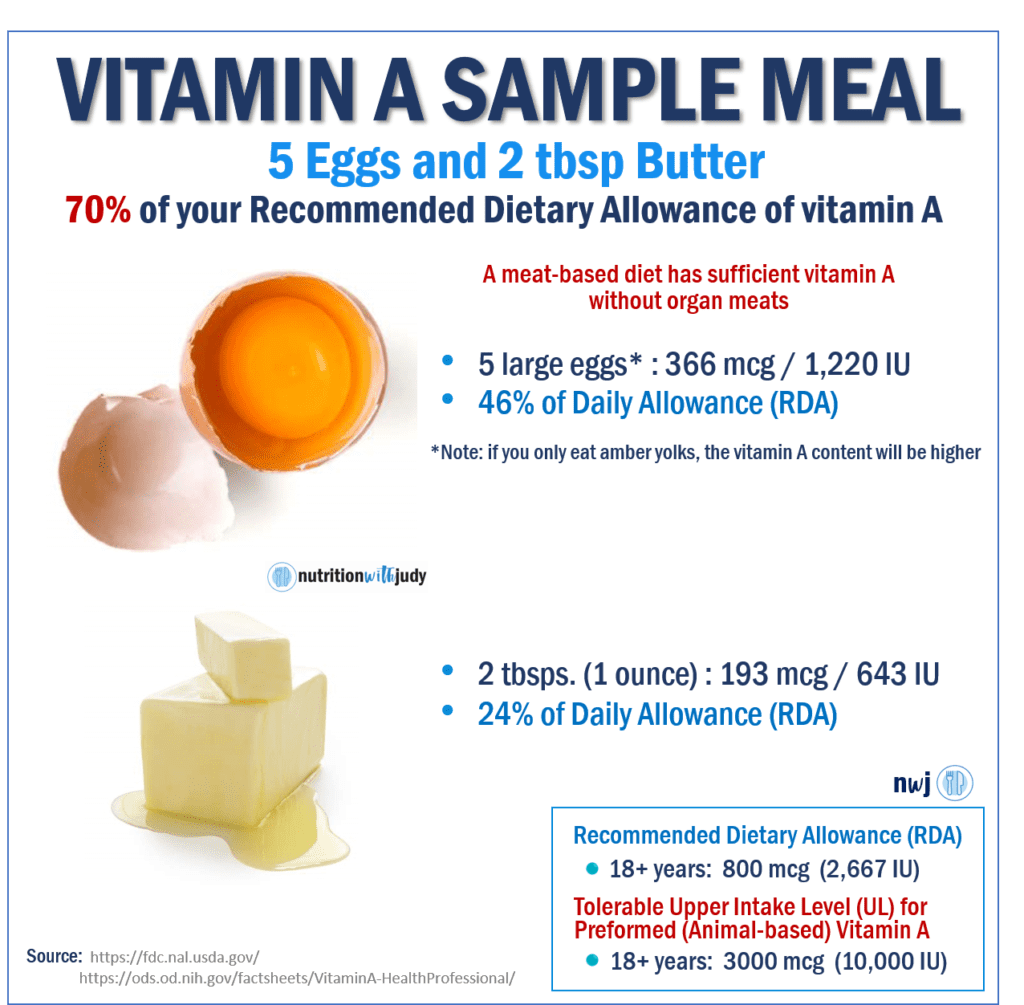
Now, this doesn’t even consider the fact that vitamin A is a fat-soluble vitamin and can accumulate in the body. If you keep consuming vitamin A foods, the liver will keep storing vitamin A. Retinol (vitamin A) has a long half-life in the body because of its hydrophobic (water-hating) nature and has a tendency to stay in fat droplets in the liver.
This holds true when vitamin A foods are consumed daily.
Polar Bear and Humans: Vitamin A
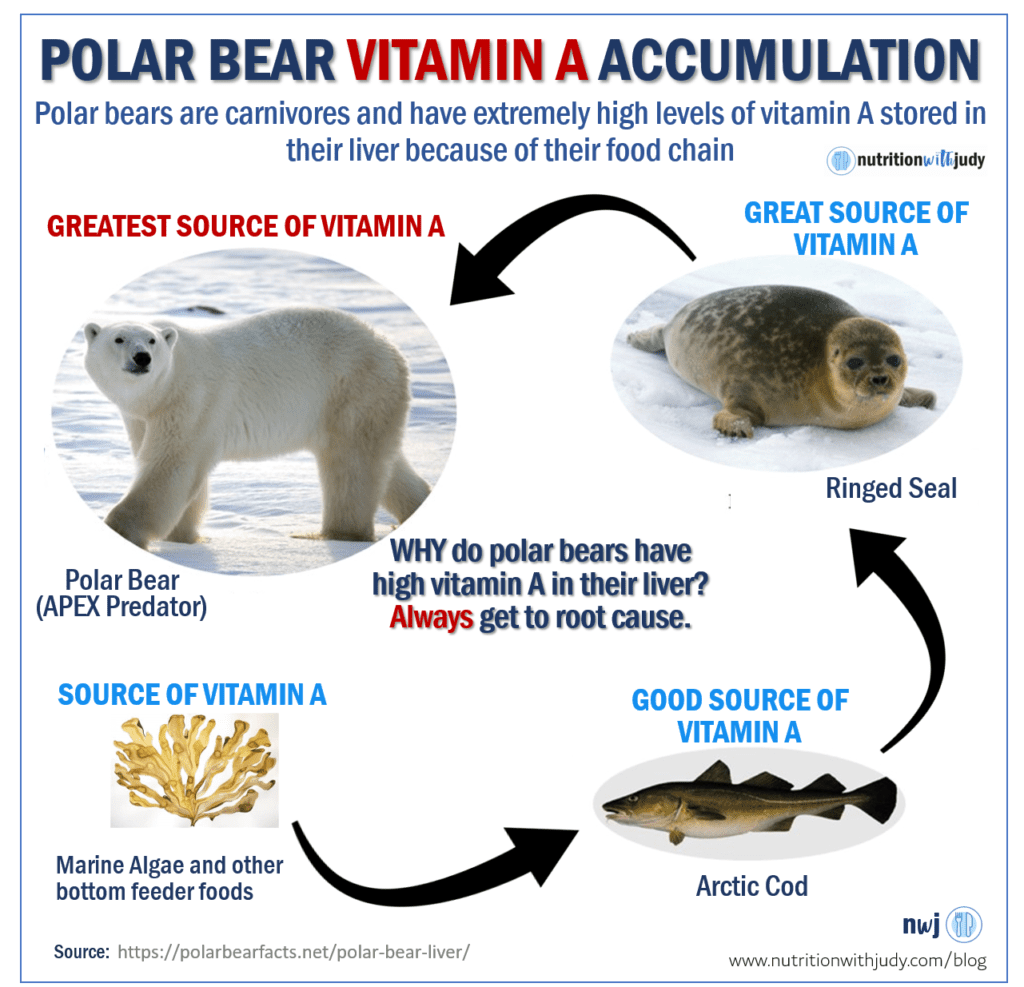
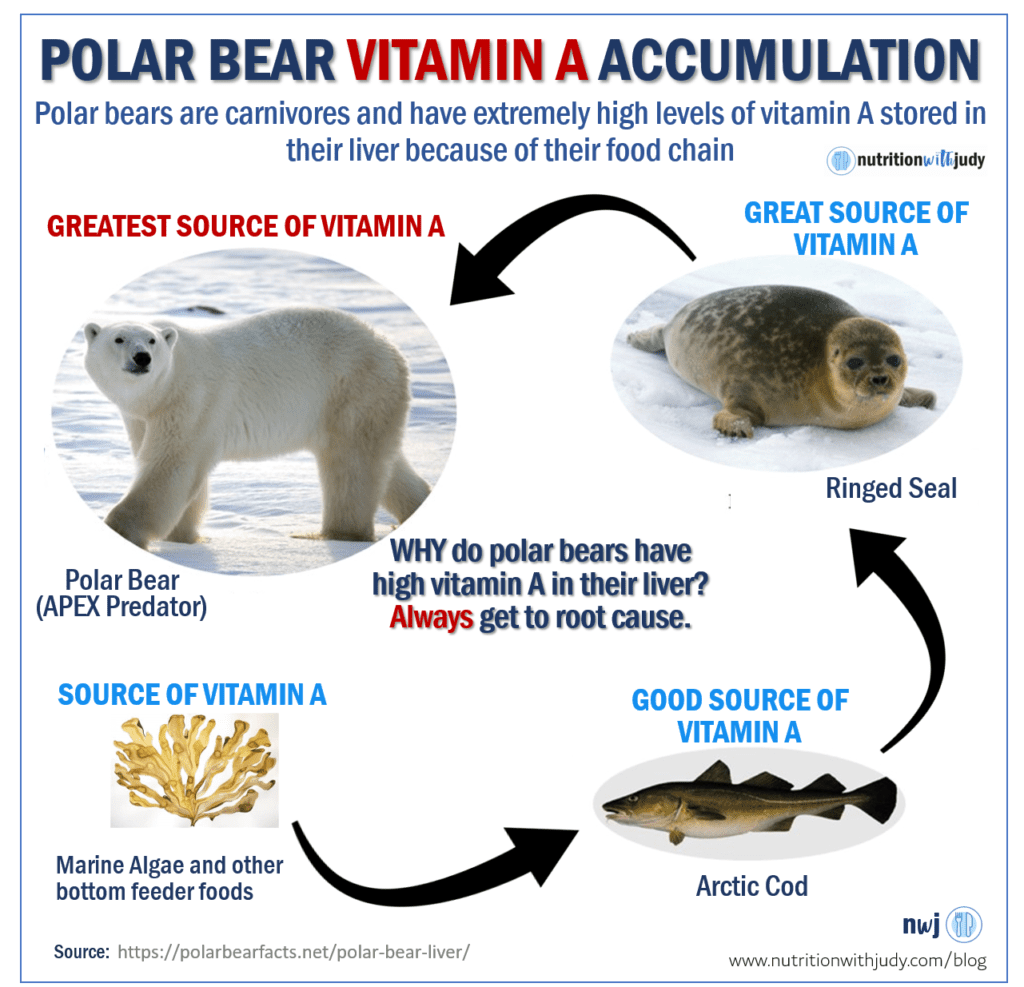
There have been many discussions about liver only causing toxicity because of its high vitamin A content. If you’ve followed my work for a while, I always talk about getting to root cause.
Well, why is the polar bear’s liver so rich in vitamin A?
Because the polar bear’s food chain has a lot of vitamin A foods. I just showed the numbers on cod liver oil. Well, imagine the seal eating lots of cod (and its cod liver oil) and then the polar bear eats many seals.
It’s obvious why the polar bear has an accumulation of high vitamin A levels. But unlike humans, polar bears can tolerate high amounts of vitamin A because that’s what nature intended.
And just to make clear, polar bears don’t consume synthetic vitamin A. Yet, they are still accumulating large amounts of vitamin A in their liver.
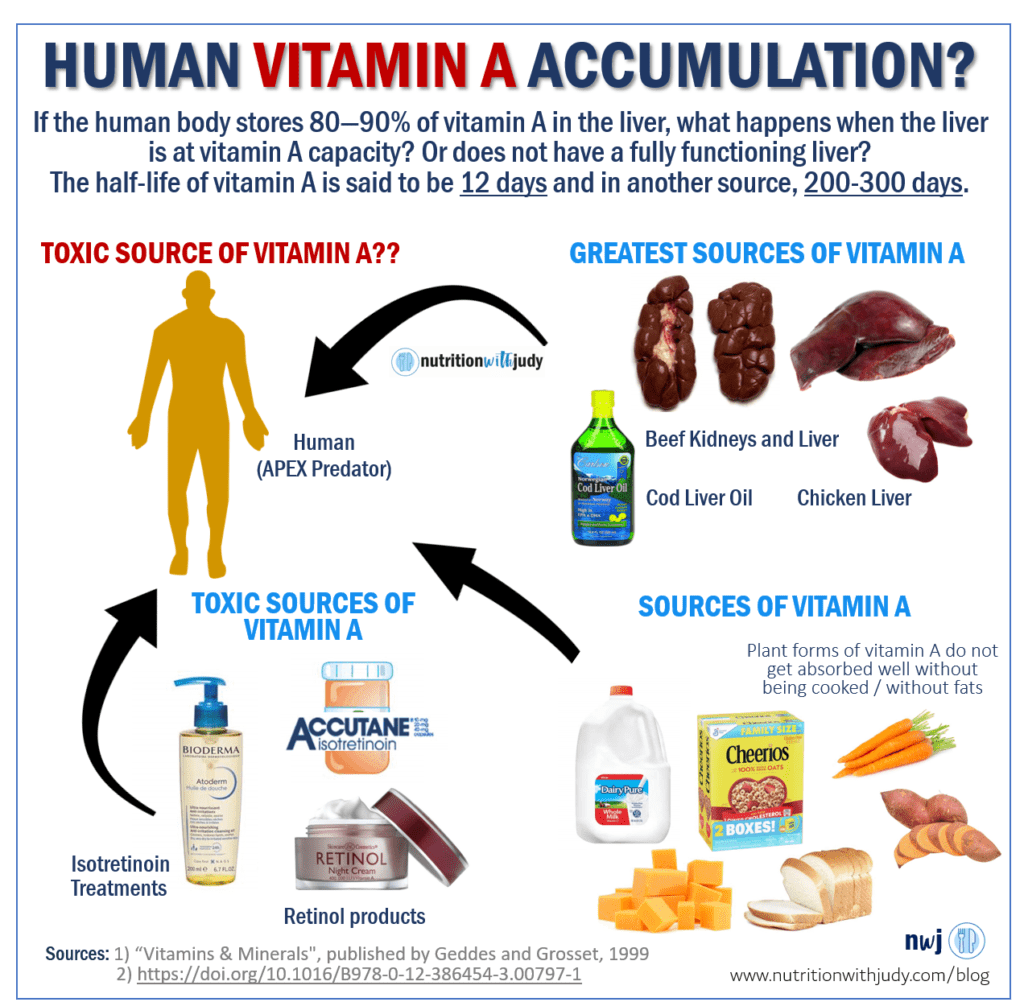
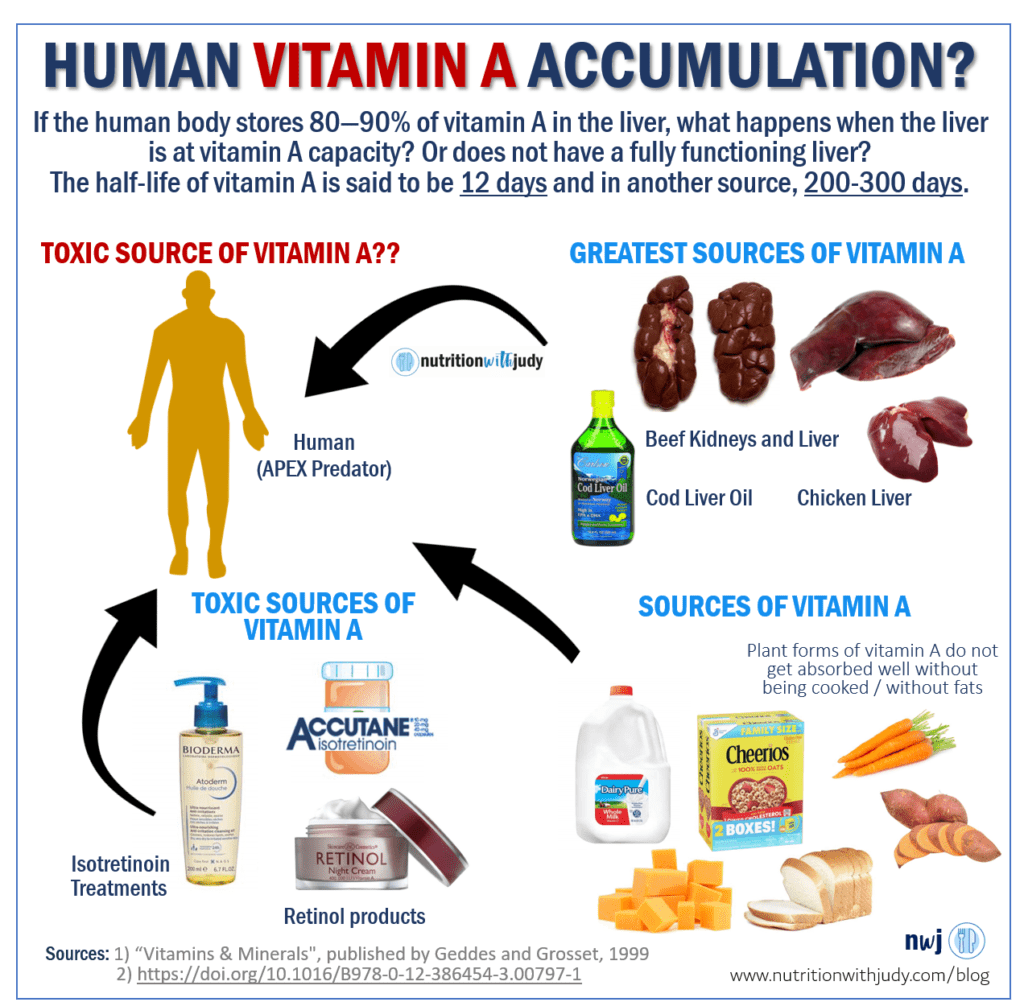
If we apply this same reasoning to humans, with all the foods and products we introduce the body to, we are likely accumulating vitamin A in the body, especially the liver. Remember, the liver stores about 80-90% of the body’s vitamin A. And if you have non-alcoholic fatty liver disease, the storage of vitamin A is impaired. You can read the study here.
The issue is that this may not be what nature intended. Humans cannot tolerate as much vitamin A as polar bears can but vitamin A is being added to everything. Even in our retinol products, suncare, and Accutane medications. And remember, vitamin A accumulates in the liver.
Some say it can take months to years to start seeing signs of vitamin A toxicity. The daily amount will matter here.
Some say it takes 1-2 years to deplete the body of vitamin A. Others say it’s shorter.
I say, why take the risk?
If you can’t absorb enough nutrients from only muscle meats or can’t eat enough variety on a meat-based diet because of food intolerances, maybe eating liver is a risky band-aid to be using daily.
Maybe the root cause solution is healing the gut and balancing minerals.
Signs of Vitamin A Toxicity
If you feel any of the following symptoms, you may just want to try an elimination diet of no liver or kidneys and even less butter and ghee for a few months. See if you feel better. This is your n=1 experiment.
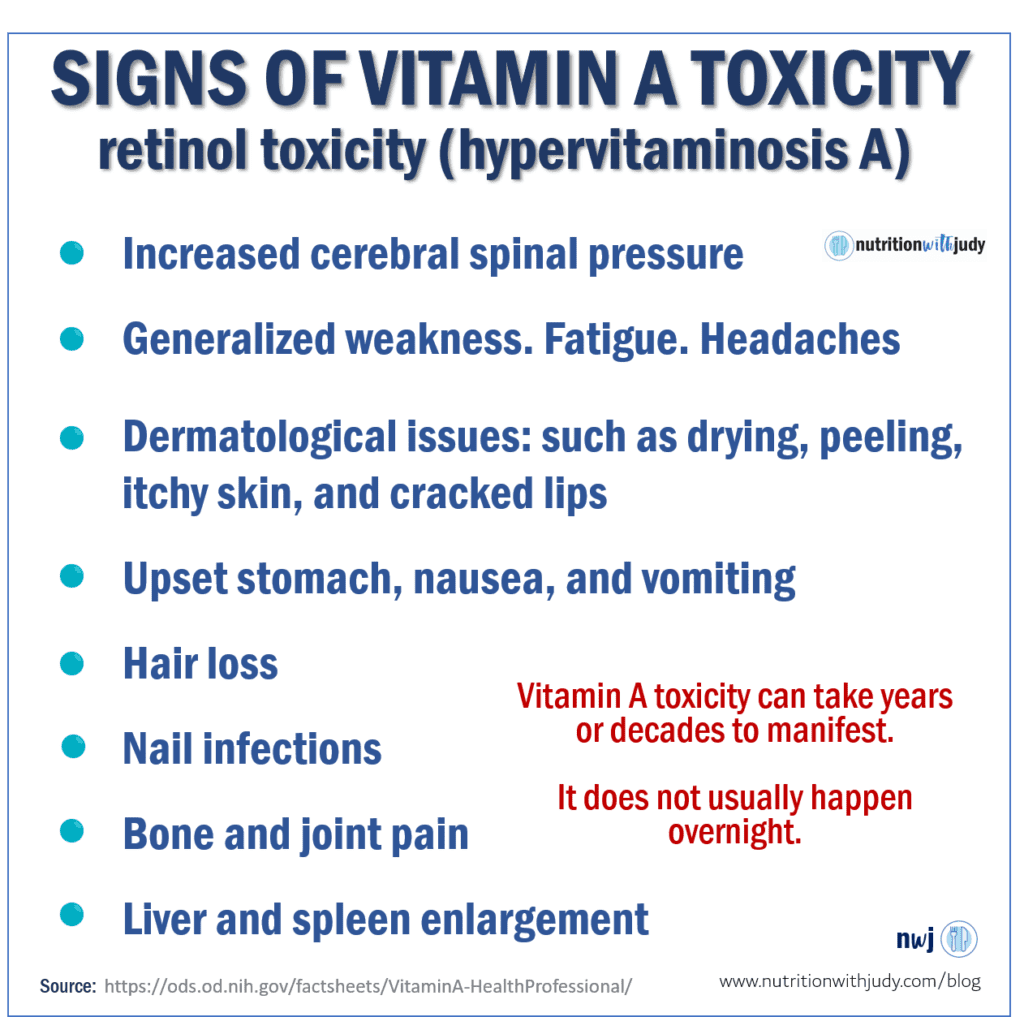
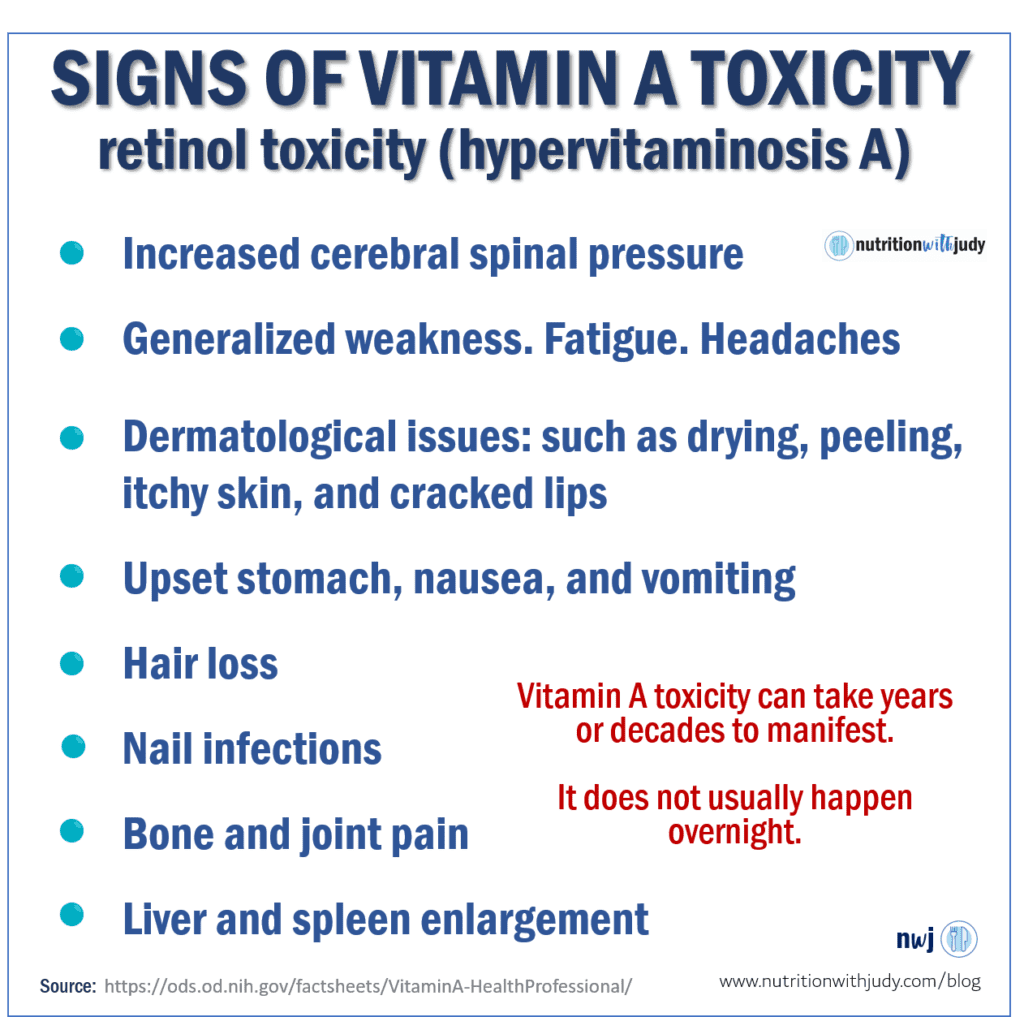
Grant Generuex also mentions checking your LDL levels. People consuming liver consistently for a year and eating meat-based may have higher LDL levels than someone eating meat-based with mostly muscle meats. You can get it checked and then eliminate all liver, vitamin A-rich products and lighten the butter and ghee-load and see if your markers improve.
Yes, LDL matters in context to HDL and triglycerides but it’s still a simple experiment that you can easily try.
In a 2018 study, one study on cadavers showed that 33% of livers biopsied had hypervitaminotic concentrations of vitamin A. This study showed that more people are vitamin A-toxic than vitamin A-deficient.
Yes, these people were not eating meat-based. But arguably with the amount of vitamin A-rich foods in a meat-based diet, I would not be surprised if more than 33% of the meat-based population that eats liver, eggs, dairy and uses retinol products have toxic vitamin A levels in their liver.
When people consume too much vitamin A, their tissue levels take a long time to decline after they discontinue their intake. And just like with oxalate cell poisoning, sometimes the resulting liver damage is not always reversible.
Consuming extremely high vitamin A foods, like liver, (especially weekly) doesn’t seem like a risk worth taking.
Testing for Vitamin A Levels
The gold standard to measure vitamin A levels in the liver is a biopsy. That is not recommended. As the blood is a carrier method for nutrients and other bodily mechanisms, the goal is always homeostasis. The blood always needs to be in a specific range for health.
This is why blood sugar levels will always be balanced until the body cannot do it any longer. Disease is imminent and it may manifest as diabetes. The same holds true with osteopenia and osteoporosis. The blood will balance calcium levels until it cannot do so any longer. Your bones will keep balancing calcium levels in the blood until disease is imminent.
This is why checking blood levels for fat-soluble vitamin status and mineral status are not always ideal.
Merck and Vitamin A Toxicity
Merck Manuals is a reference guide for physicians and pharmacists and they discuss the following vitamin A toxicity risks:
- Adults who consume >1500 mcg/day of vitamin A may develop osteoporosis.
- Infants who are given excessive doses of 6,000 to 20,000 (mcg/day) if vitamin A may develop toxicity within a few weeks.
- Birth defects occur in children of women receiving isotretinoin (related to vitamin A) for acne treatment during pregnancy.
- Megadoses of vitamin A can cause liver toxicity.
Closing Thoughts
Since you can’t really do a liver biopsy, you can always try removing liver and kidneys for several months and see how you feel. You can then add them back slowly and see if anything improves or worsens. Following the Carnivore Cure elimination and reintroduction protocol will help you navigate this process.
If you have used zero skincare products that use retinol and don’t consume any dairy or eggs, beef liver may be okay for you. I would still choose the real food varieties of liver to let your body guide you.
Try the Coca’s Pulse test to see how your body responds.
Ultimately, you have to find what makes sense for you. I hope this information helps you make a better-informed decision, especially if a meat-based diet isn’t helping you feel better. I hope this share brings you an understanding of the implicated risks with consuming liver daily or even weekly.
Additional Resources
If you want to watch the Grant Genereux interview, you can find it here as a podcast, or here as a YouTube video. I will be sharing more interviews on this topic so that you can ultimately make a better-informed, individual-specific decision.
I also shared my honest thoughts and why I even decided to share all the info in a very personal Cutting Against the Grain podcast episode here.
If you are wondering what to eat on a meat-based diet, I wrote a “Don’t Eat Just Beef” blog post a while ago (still need to update the recommendation for chicken liver). The blog post will give you an idea of how to better cover nutrient density on a meat-based diet. You can read it here.
Some of us don’t consume dairy and eggs, and consuming liver may make sense. But for those that were forcing it down for its nutritional value, even when they didn’t feel well, I shared this for you.
For some, liver and kidneys are nutrient-dense foods but for some, it’s not an ideal food. For not having enough insight, I apologize for giving a broad-brushed answer of liver’s health benefits without considering the risks.
I hope my sharing now can do some healing.
w️ith ♥ and hope for healing,


If you enjoyed this blog post, you may also enjoy these Nutrition with Judy blog posts:
- Written Interview with Chris Masterjohn and Liver
- Don’t Eat Just Beef on a Meat-Based Diet
- Make Meat a Priority for You and Your Children
- What’s in Canola Oil
- Meat and Climate Change
DISCLAIMER: The content is for educational purposes only. While I am a nutritional therapy practitioner, I am not providing medical advice. Whenever you start a new diet or protocol, always first consult with your trusted practitioner.
REFERENCES
- Nutrition with Judy + Grant Genereux Podcast Interview
- Nutrition with Judy + Grant Genereux YouTube Interview
- Cutting Against the Grain Podcast: Judy + Laura’s Take on Liver and Ancestral Eating
- Interview with Chris Masterjohn on Consuming Liver
- Grant Genereux
- https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional/
- https://pubmed.ncbi.nlm.nih.gov/30265402/
- https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency-dependency-and-toxicity/vitamin-a-toxicity
- https://pubmed.ncbi.nlm.nih.gov/833680/
- https://pubmed.ncbi.nlm.nih.gov/10424294/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1258540/
- https://www.ncbi.nlm.nih.gov/pubmed/19153339
- https://sciencebasedmedicine.org/vitamins-and-cancer-risk/
- http://sciencenordic.com/confirmed-vitamin-pills-can-cause-death
- https://www.acpjournals.org/doi/10.7326/0003-4819-129-10-199811150-00003
- https://academic.oup.com/ajcn/article/83/2/191/4649798
- http://a2zproject.org/~a2zorg/pdf/2final.pdf
- http://www.a2zproject.org/~a2zorg/pdf/Vitamin%20A%20fortification%20of%20wheat%20flour%20Considerations%20and%20current%20recommendations.pdf
- https://www.academia.edu/1245487/Vitamin_A_Fortification_of_PL480_Vegetable_Oil
- https://www.dairynutrition.ca/nutrients-in-milk-products/other-nutrients/why-is-vitamin-a-added-to-milk
- https://www.who.int/elena/titles/vitamina_fortification/en/
- https://pubmed.ncbi.nlm.nih.gov/15001122/
- https://pediatrics.aappublications.org/content/113/Supplement_3/1097
- http://www.vitaforum.net/old/newsletters/0103/articles/doc0033.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6692705/
- https://fdc.nal.usda.gov/fdc-app.html#/food-details/169451/nutrients https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6692705/
- https://www.sciencefocus.com/the-human-body/will-you-die-if-you-eat-a-polar-bears-liver/
- https://pubmed.ncbi.nlm.nih.gov/29286303/
- https://academic.oup.com/ajcn/article/83/2/191/4649798
- https://www.semanticscholar.org/paper/Natural-Antioxidant-Use-in-Ghee-A-Mini-Review-Hazra-Parmar/1eb229038973eb241e08740c1abd70c987a87e99?p2df
- https://www.webmd.com/diet/liver-good-for-you
- https://www.instagram.com/p/B51K0qFlNqL/
- https://drgundry.com/dr-terry-wahls-transcript/




Noaddedsugar
May 15, 2021 at 6:52 amThank you so much. Totally explains my hair falling out. Totally explains why I felt all of the above symptoms and why I generally felt like crap on my carnivore way of eating. Yes, I was taking liver capsules, loads of butter, eggs, very little muscle meat and using retinol on my skin daily. I will need to re-focus and get on to your carnivore cure Judy. I used to watch you on Youtube before watching many well-meaning carnivore diet ‘experts’. I got lost and confused by so many different opinions.
VALERIE
May 16, 2021 at 6:17 pmWOW! Thank you so much, Judy, for your generous posting of this important material from your excellent book.
Viktor
November 20, 2021 at 5:39 amThanks so much for this. Here’s my story:
Male, 31 as of November 2021.185 cm, ~ 76 kilos. Born and living in Moscow, Russia.
From childhood, I always was what you may call a “nerdy” type of boy – pale, skinny, not into any kind of sports, liked PC games and movies, hated physical education lessons at school. Had quite a lot of friends, but our mutual interests revolved more around virtual worlds and school subjects, rather than any recreational sports.
A short time after getting into university, I started to attend swimming pool lessons, as well as the gym. And that was the start of my progress from the definitive nerd into being quite a fit and muscular guy. I had two swimming sessions a week as part of my university Physical Education practice, and also hit the gym three times a week. I started eating healthier, though consumed a bit of alcohol during my first semesters, but then dropped it and haven’t had a drink for almost 8 years by now, I guess.
All in all, I was training religiously, swimming for a couple years, and eating as healthy as I could think of and possibly afford (I mean the usual “fitness” stuff to gain muscle: dairy, meat, a bit of fish, eggs, whole grains, nuts, fruit, veggies, etc). I put on several kilos of nice muscle mass and was even considered “beefy” by some friends.
Then I heard about all of the supposed benefits of the vegetarian diet I decided to give it a try. And this is where I must make a very important point about myself – when I’m focused on something or committed to an idea, it really takes hold of me. It’s like when I’m into a diet, or a new trend, you can be sure it’s 101%. It’s a very bad character trait as I now realize.
So I went on with avoiding meat/fish for some time and then switched to the more extreme vegan diet after reading the (in)famous China Study (no offense to any vegans here, it’s just my experience). I would eat lots of nuts, seeds, whole grains, legumes, oils, fruit, veggies, tofu, and talking b12 supplements. However, I wasn’t able to sustain it for very long as I gradually became sluggish, caught an illness almost every week, my hemoglobin dropped to the lower range of normal, and as I was also donating blood every other month and wasn’t going to stop it, the vegan diet had to go. So, I went back to eating eggs and dairy, and then added meat and fish. I started to feel better almost in a matter of days, as far as I remember.
Being a health-obsessed jerk by that time as I was, I was looking for more nutritious foods to incorporate into my daily diet. Seaweed, more varieties of nuts, seeds, and, you guessed it, beef and chicken liver, one of the most nutrient-packed things one can ever eat. Do you remember how quickly I could become too obsessed with something? So liver was no exception, and what’s not to like about it? It’s dirt cheap, extremely nutritious, and was even to my taste (not that being not-so-tasty would ever discourage me from eating something if that was healthy food).
In 2017-2018 I ate maybe around 500 grams a week and then increased it to two 500g packs of chicken liver pan-fried with onions per week. Also, I didn’t forget eggs, dairy, and then started to incorporate canned fish liver (very oily) as well, not even knowing about its very high vitamin A content. I took some sports vitamin complex as well, which also must have contained quite a lot of vitamin A.
My first symptoms were very dry and cracked skin on my palms, and the cracks and blisters from working out and doing pull-ups had a very noticeable yellow color. I googled if one could have vitamin A toxicity from eating liver and most sources said that one could get it in theory, but if consumed in moderation, liver is okay and very healthy. I never counted the vitamin A content of all the food I was consuming, and even a kilo or more of chicken or beef liver didn’t seem that much when spread over a week. So basically I just continued.
Other symptoms became more troublesome over the next months to a year – very flaky sculp, anxiety, sleep disturbances (which I decided was due to overtraining, that was also a thing with my fitness obsession), terrible mood swings, bladder irritation, reflux and sensitivity to foods that were all okay before, dry eyes to the point that cutting onions (when making pan-fried liver, of course!) would cause them to sting and be irritated, but didn’t bring any tears at all.
Fast-forward a few more months, I became really sluggish, brain fog was unbearable at times, very sensitive to cold, constipated, depressed, and irritable. I tried intermittent fasting, took vitamin D supplements and kelp iodine pills, was tested (and treated by some docs) for supposed parasites, candida, but there was no apparent improvement. I tried to keep a regular workout schedule, eat healthier, added kale, broccoli, and lots of carrots, which only seemed to add insult to injury. By that time I stopped dairy as I could no longer tolerate it.
I developed carotenemia on my face, palms, and feet. I didn’t know what it was at that time, only understood that it wasn’t jaundice as the eyes were white and normal-looking. The docs suggested I get tested for viral infections (yeah, in a person who was a blood donor not too long ago and got tested on every donation), get a liver ultrasound and liver enzymes tested, but all that was normal.
My labs showed a consistent pattern – very high cholesterol (7-8.8 mmol/L), high blood calcium, elevated histamine, normal liver enzymes, low WBC (which was almost definitely a result of all the stress and overtraining), normal TSH (always!) but borderline low free T4 and low T3.
When from one GI doc to another, and then to various endocrinologists, but they all turned a blind eye to the whole picture and treated only the symptoms within their purview.
Then something almost miraculous happened one day when I decided not to eat my usual carrot-and-apple salad for breakfast and also to forgo boiled carrots as a side dish for lunch. After only a couple of days on this new “diet” to me, my symptoms greatly improved. I could think and see things clearly for the first time in months. I had energy; I wanted to take a walk, to do things, to read something, etc. Then, after a couple of weeks of steady progress, I f**d this up by adding more dairy, especially cheese, and a bit of high b-carotene foods to my diet. My palms became yellowish again (although not nearly as much as from carrots previously), digestion worsened, and the progress seemed to come to a halt.
However, I already knew that I had some issues with beta-carotene, so now the problem was easier to dig into. I read some forums and stumbled upon people with almost exactly the same stories, and also found published papers on vitamin A toxicity from eating liver. Now I’m planning to steadily recover as I’ve seen quite a lot of improvement over the last week after starting to pay attention to my diet regarding vitamin A and b-carotene.
Truth59
July 22, 2023 at 7:35 amSo if I’m taking six liver caps/day I might not need my CLO.